Diabetes:华人学者发现二甲双胍治疗肥胖相关糖尿病的新机制
2016-06-13 佚名 生物谷
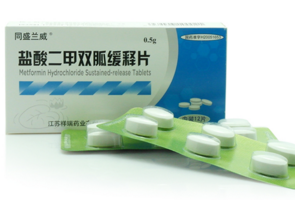
近日,美国波士顿大学医学院华人学者Mengwei Zang领导的研究小组在国际学术期刊Diabetes上发表了一项最新研究进展,他们发现抗糖尿病药物二甲双胍能够抑制白色脂肪组织发生纤维化,从而改善胰岛素抵抗,并对其中机制进行了深入研究。在肥胖疾病中,脂肪纤维化逐渐成为白色脂肪组织发生代谢紊乱的一个标志。脂肪组织纤维化会损伤脂肪细胞的可塑性,但是目前对于肥胖发生过程中白色脂肪组织如何发生细胞外基质的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#DIA#
27
#BET#
39
#Diabetes#
35
#华人#
35
#华人学者#
33
?
131