Nat Commun:原发性肝癌肺转移存在骤变拐点, CALML3基因可抑制肝癌生长和肺转移
2018-04-10 钟萱 复旦大学附属中山医院
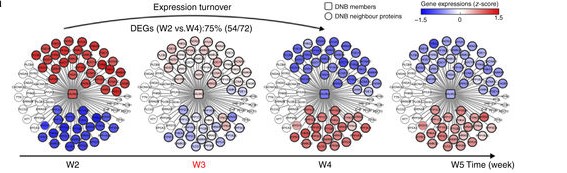
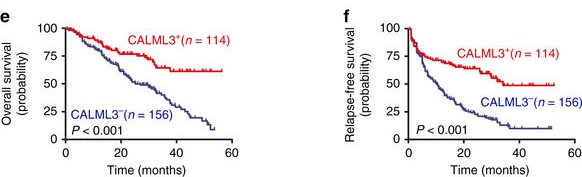
近期,复旦大学附属中山医院肝肿瘤内科夏景林教授与中科院细胞生化所陈洛南研究员课题组进行合作,首次成功鉴定肝癌肺转移发生前的临界阶段,发现原发性肝癌肺转移存在骤变拐点,并首次报道了钙离子传导蛋白(calmodulin-like-protein,简称CALML3)可抑制肝癌生长和肺转移。相关研究成果以“Dynamic network biomarker indicates pulmonary meta
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#COMMUN#
24
#Nat#
34
#原发性#
30
#拐点#
34
学习了谢谢分享!!
66
#原发性肝癌#
40
#肺转移#
27