JTO:克唑替尼治疗的ALK重排NSCLC患者的长期结局如何
2017-06-14 陶白 肿瘤资讯
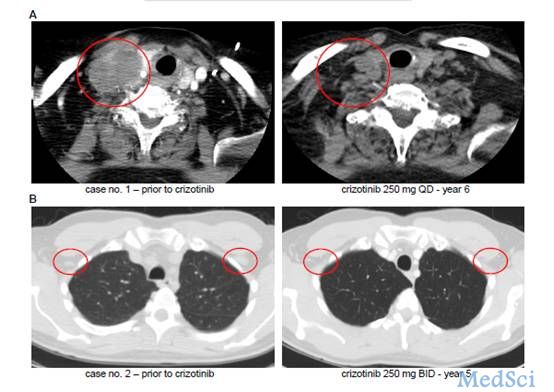
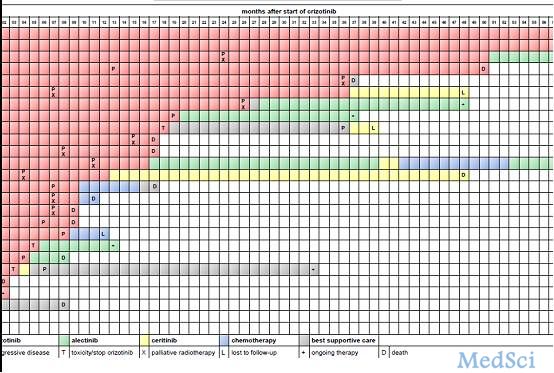
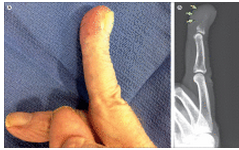
许多研究显示,克唑替尼对ALK重排的NSCLC患者有效,但是更长期的患者结局却鲜有报道。美国贝斯以色列女执事医疗中心血液学/肿瘤学科的Daniel B. Costa博士报道了两例ALK重排的NSCLC病例的5年PFS和OS,并回顾性审查了该中心的ALK FISH检测阳性病例,相关研究结果6月2日已被《JTO》所接收。

Journal of Thoracic Oncology.DOI: http://dx.doi.org/10.1016/j.jtho.2017.06.002
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#SCLC患者#
0
#长期结局#
43
#NSCLC患者#
35
间变性淋巴瘤的接抗剂
60
药物治疗取得这种效果不错了
59
学习了,谢谢分享
46
学习了,谢谢分享!
59
谢谢分享
62