Stroke:如何降低颈动脉内膜切除术的风险?
2017-03-14 MedSci MedSci原创
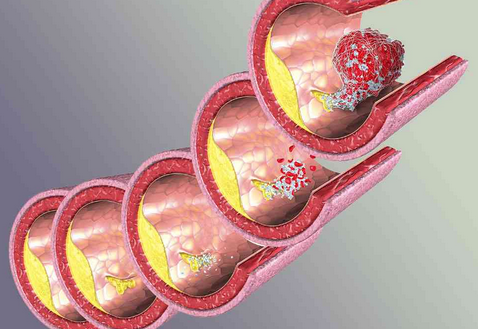
在德国,所有关于颈动脉分叉的手术和血管内手术必须记录在法定的全国质量保证数据库中。近期,一项发表在杂志Stroke上的研究旨在分析颈动脉内膜切除术后程序性和围手术期变量与院内卒中或死亡率之间的关联。此项研究选取2009年至2014年之间,数据库中记录的无症状或有症状颈动脉狭窄的142074例选择性颈动脉内膜切除手术患者。二次数据分析的主要终点是住院卒中或死亡。通过多变量多层回归分析评估调整的相对风
在德国,所有关于颈动脉分叉的手术和血管内手术必须记录在法定的全国质量保证数据库中。
近期,一项发表在杂志Stroke上的研究旨在分析颈动脉内膜切除术后程序性和围手术期变量与院内卒中或死亡率之间的关联。
此项研究选取2009年至2014年之间,数据库中记录的无症状或有症状颈动脉狭窄的142074例选择性颈动脉内膜切除手术患者。二次数据分析的主要终点是住院卒中或死亡。通过多变量多层回归分析评估调整的相对风险(RR)。
此项研究的主要结果发生在1.8%的患者中,无症状患者的发生率为1.4%,有症状患者的发生率为2.5%。在多变量分析中,较低的中风或死亡风险与局部麻醉独立相关(与全身麻醉相比:RR,0.85; 95%置信区间[CI],0.75-0.95),颈动脉内膜补片成形术与初级闭合术相比(RR,0.71; 95%CI,0.52-0.97),通过双重超声(RR,0.74; 95%CI,0.63-0.88)或血管造影术(RR,0.80; 95%CI,0.71-0.90)的术中完成研究以及围手术期抗血小板药物治疗(RR,0.83; 95%CI,0.71-0.97)。没有分流和短的交叉钳位时间也与较低的风险相关。
此项研究得出结论:与初级闭合术相比,局部麻醉、补片成形术,通过双重超声或血管造影术中完成研究和围手术期抗血小板药物与较低的院内卒中或死亡率独立相关。
原始出处:
Knappich C, Kuehnl A, et al. Intraoperative Completion Studies, Local Anesthesia, and Antiplatelet Medication Are Associated With Lower Risk in Carotid Endarterectomy. Stroke. 2017 Mar 10. pii: STROKEAHA.116.014869. doi: 10.1161/STROKEAHA.116.014869.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#内膜#
34
#颈动脉#
27
#切除术#
26
学习了,很有用
66