临床医生如何正确理解和解读超声心动图报告
2015-04-08 张天龙(北京朝阳急诊抢救中心 即时超声
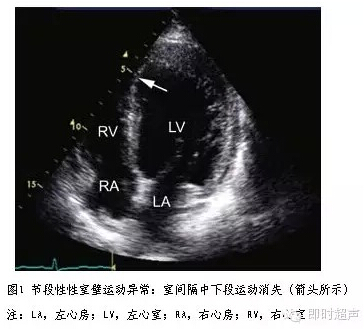
节段性室壁运动异常是否等同冠心病 超声心动图常被用于评价心脏的局部室壁运动异常来探查已知的或可疑的冠心病。缺血的心肌超声心动图表现为室壁运动减弱或消失或反常运动,心肌梗塞后或慢性心肌缺血引起心肌纤维化和疤痕形成,心肌节段回声密度增加,运动消失,舒张期室壁厚度也变薄。对于缺血性心脏疾病来说,这种节段性室壁运动异常是急性、慢性心肌缺血和心肌梗塞的共有特征。二维超声心动图显示的节段
节段性室壁运动异常是否等同冠心病
 这里,LVEDV=左室舒张末容积;LVESV=左室收缩末容积。
推荐的根据左室射血分数对左室功能进行分级的参考值见表。
这里,LVEDV=左室舒张末容积;LVESV=左室收缩末容积。
推荐的根据左室射血分数对左室功能进行分级的参考值见表。 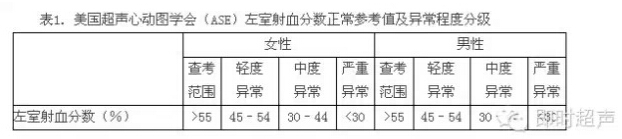
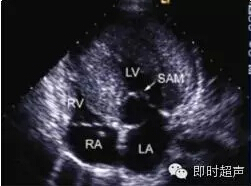
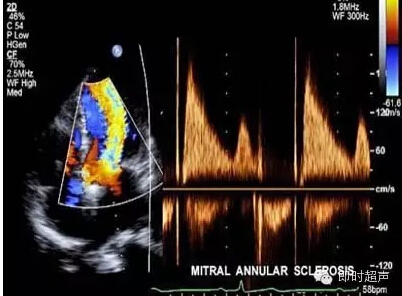
从以上的计算公式中可以看出,LVEF实际上是反映左室舒张末期和收缩末期容量的变化比率,因此,收到容量负荷的影响较大。在实际临床工作中,要结合患者的临床情况和心脏病变对左室射血分数进行理解和解读。例如在肥厚型心肌病的患者,由于左室肥厚导致左室腔变小,如果左室舒张末期容量60ml,收缩末期容量30ml,每搏量30ml,LVEF为50%。对于中至重度二尖瓣反流的患者,如果左室舒张末期容量为150ml,收缩末期容量为75ml ,每搏量75ml,LVEF为50%。 临床上LVEF均为50%,但是每搏量确差别很大,因此后者的症状可能较前者要轻。另外左室射血分数可能不是反映左室心肌收缩性能的适当指标,当中至重度二尖瓣反流患者出现名义上正常的60%的左室射血分数时,其左室收缩性能可能已经处于不正常状态。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













不错哦
143
很不错!受教了!
122
#心动图#
37
学到新东西了,谢谢
129
太有价值了
119
看完更清晰了,有了新认识
132
必须要接受教育、认可理念
57
必须要接受教育、认可理念
69
临床医生太依赖辅助科室了
89
#临床医生#
35