Injury:改进后的PFNA-II治疗不稳定型转子间骨折安全有效
2014-11-12 虎群盛 丁香园
由于骨质疏松所导致的股骨转子间不稳定型骨折对于骨科医生来说是一种挑战,具有较高的治疗失败率和并发症发生率。从解剖学形态上看,和欧美人种相比,中日韩等亚裔老年人存在股骨颈更短、颈干角更小、股骨前弓更大等特点,因此使用标准的股骨近端髓内钉PFNA时容易出现与之相关的内固定断裂、螺钉穿出、股骨干骨折等问题。亚洲版防旋型股骨近端髓内钉PFNA-II在螺钉设计上进行了一些改进,如:主钉近端的直径从1
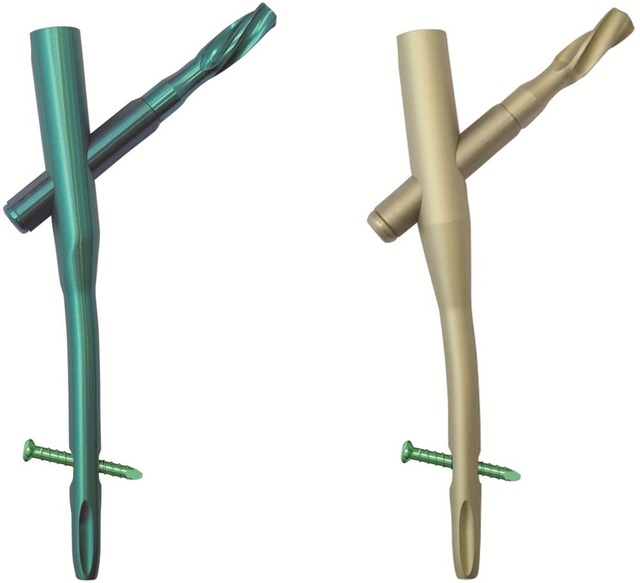
由于骨质疏松所导致的股骨转子间不稳定型骨折对于骨科医生来说是一种挑战,具有较高的治疗失败率和并发症发生率。从解剖学形态上看,和欧美人种相比,中日韩等亚裔老年人存在股骨颈更短、颈干角更小、股骨前弓更大等特点,因此使用标准的股骨近端髓内钉PFNA时容易出现与之相关的内固定断裂、螺钉穿出、股骨干骨折等问题。亚洲版防旋型股骨近端髓内钉PFNA-II在螺钉设计上进行了一些改进,如:主钉近端的直径从17mm缩小到16.5mm,螺旋刀片的直径从10.55mm缩小到10.3mm,主钉外翻角从6°减小到5°,主钉远端扁平化设计(见图1)。

图1 PFNA-II(左)与PFNA(右)的比较
日本的学者Takeshi Sawaguchi使用亚洲版PFNA-II治疗老年骨质疏松性股骨转子间骨折取得了良好疗效,其研究结果发表在2014年10月的Injury杂志。
作者收集统计20家医院的176例使用PFNA-II治疗的65岁以上不稳定型股骨转子间骨折日本患者(AO分型31-A2或31-A3),患者在受伤7天内手术治疗。排除病理性骨折、其他肢体骨折、麻醉评分V或VI、长期卧床、酗酒、既往髋部骨折、以及存在严重精神疾病的患者。
患者的平均年龄为84岁(67-98岁),女性占76%(133/176),A2型骨折152例,A3型骨折24例,平均身高体重指数为20.8,66%的患者身高体重指数正常,但也有25%的患者体重偏轻或过轻。97例患者(55%)通过测量对侧股骨骨密度而确诊骨质疏松。
最主要使用的PFNA-II的长度为170mm,占79%,70%所用钉子的远端直径为9或10mmm。所有的骨折均愈合,87%的患者愈合时间在12周以内。
共发生3例术中内固定并发症,在术后1年随访期间还有另外15例与内固定有关的并发症。有一例患者发生了1次术中和2次术后并发症,因此被计为一例。术中内固定并发症的发生率为1.7%(3/176),术后并发症的发生率为8%(14/176)。术中3例并发症包括2例术中骨折复位不良和1例远端锁定钉出现的问题。术后并发症主要包括股骨颈短缩超过5mm(8例)和内固定断裂(3例)。
3例术中并发症以及5例术后并发症主要与手术技术相关。术后内固定断裂的情况包括:1例A3.3型骨折术后负重后出现远端横行锁定钉孔处断裂,给予限制负重后骨折愈合;另外一例A3.3型骨折在术后3个月时远端横行锁定钉孔处断裂,进行翻修手术更换为长钉后4个月骨折愈合;第三例为影像学上发现的远端锁定螺钉断裂,但患者并无任何临床不适。15例术后并发症的患者中只有3例患者需要再次手术。
统计学分析显示:并发症的发生与性别、年龄、初始螺旋刀片位置、术者经验、身高体重指数之间并无显著联系。A3型骨折患者发生内固定并发症的风险是A2型患者的2.9倍。
导致出现内固定并发症的主要原因是“骨骼/骨折”因素(9/14)。17例患者(10%)存在影像学上的植入物与股骨髓腔内侧皮质的接触(不匹配)。其中11例(65%,11/17)为髓内钉远端与股骨内侧接触,还有4例患者为多个部位的不匹配。

图2 PFNA-II可能与股骨近端不匹配的地方:1 髓内钉的近端外侧部分,2 髓内钉中间部分与髓腔的内侧皮质 3和4 髓内钉的远端
因此作者认为:经过改进后的亚洲版PFNA-II对于不稳定型股骨转子间骨折患者安全有效,但是改进后的髓内钉仍与股骨存在一定程度的不匹配。
原始出处
Sawaguchi T1, Sakagoshi D2, Shima Y3, Ito T4, Goldhahn S5.Do design adaptations of a trochanteric nail make sense for Asian patients? Results of a multicenter study of the PFNA-II in Japan.Injury. 2014 Oct
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Injury#
45
#FNA#
40
#转子间#
30
#稳定型#
26
#PFNA-II#
32