ASO:临床N分期结果为口腔鳞状细胞癌患者结局独立预测因素
2013-07-26 ecoliDH5 dxy
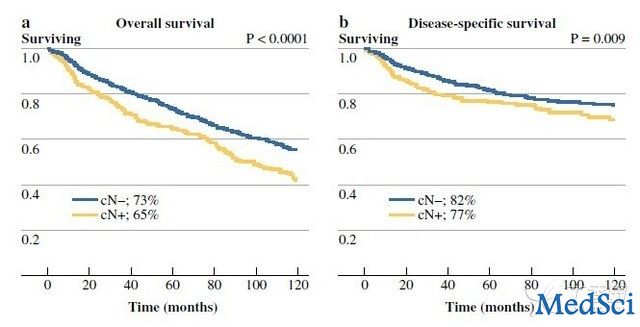
患者OS与DSS结局比较 在2013年6月18日在线出版的《外科肿瘤学年鉴》(Annals of SurgicalOncology)杂志上,发表了以色列海法Rambam医学中心Ziv Gil博士等人的一项研究结果,该文针对颈部淋巴结病理结果呈阴性(pN-)的口腔鳞状细胞癌(OSCC)患者亚群,旨在对临床N分类(cN)的意义进行研究。该研究发现,即便对于淋巴结呈pN-的患者,颈部转移的临床实证也仍
在2013年6月18日在线出版的《外科肿瘤学年鉴》(Annals of SurgicalOncology)杂志上,发表了以色列海法Rambam医学中心Ziv Gil博士等人的一项研究结果,该文针对颈部淋巴结病理结果呈阴性(pN-)的口腔鳞状细胞癌(OSCC)患者亚群,旨在对临床N分类(cN)的意义进行研究。该研究发现,即便对于淋巴结呈pN-的患者,颈部转移的临床实证也仍是患者结局的独立预测因素。
该研究共包括11个癌症中心的2,258例患者,这些患者均因OSCC接受了颈部淋巴结清扫(1990-2011),结果显示为pN-。研究中位随访时间为44个月。研究人员通过Kaplan-Meier法计算得出患者5年总生存率(OS)、疾病特异性生存率(DSS)、无病生存率、局部控制率、局局部区域控制率及远端转移控制率。此外,通过多变量分析对cN划分、肿瘤、淋巴结、转移划分系统等分期变量进行了考察。
最后共有345例患者在术前被认定为cN+,1,913例患者为cN-。结果表明,cN-患者5年OS及DSS分别为73.6及82.2 %。cN+患者5年OS及DSS分别为64.9及76.9 %。在不考虑治疗、侵犯深度或颈部淋巴结清扫范围的情况下,cN+结果为较差OS 及DSS的显著预测因素。cN分类结果与无复发生存率及局部区域(颈部及原发肿瘤)控制率有关,但与局部(p= 0.19)及远端复发率无关。

Amit M, Yen TC, Liao CT, Binenbaum Y, Chaturvedi P, Agarwal JP, Kowalski LP, Ebrahimi A, Clark JR, Cernea CR, Brandao SJ, Kreppel M, Zöller J, Fliss D, Bachar G, Shpitzer T, Bolzoni VA, Patel PR, Jonnalagadda S, Robbins KT, Shah JP, Patel SG, Gil Z; The International Consortium for Outcome Research (ICOR) in Head and Neck Cancer.Clinical Nodal Stage is a Significant Predictor of Outcome in Patients with Oral Cavity Squamous Cell Carcinoma and Pathologically Negative Neck Metastases: Results of the International Consortium for Outcome Research.Ann Surg Oncol. 2013 Jun 18. [Epub ahead of print]PMID:23775408
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ASO#
28
nn Surg Oncol. 2013
93
#细胞癌#
25
#预测因素#
26
#口腔鳞状细胞癌#
33
#患者结局#
32