Front Oncol:高危因素是dMMR/MSI-H II期结肠癌的预后因素
2021-10-30 yd2015 MedSci原创
研究表明,高危因素是dMMR/MSI-H II期结肠癌的预后因素。并且辅助化疗可以改善≥65岁高危dMMR/MSI-H II期结肠癌患者预后。
结直肠癌是常见的恶性肿瘤之一。约28%的结肠癌(CC)患者在发病时为II期。II期CC患者的风险分层依赖于分子和临床病理特征。高危因素的预后作用已被确认,如T4期、肠梗阻、组织学差/未分化、淋巴血管、神经周围浸润和<12个淋巴结。微卫星稳定II期CC患者伴有高危因素增加了癌症复发的风险和预示添加辅助治疗的益处。与IIIa期肿瘤患者相比,T4分期的II期CC患者的生存率更差。辅助化疗可改善III期CC的无进展生存期(PFS)和总生存期(OS)。II期CC的辅助治疗获益相对较小,因此并不是常规推荐。大约15%的结直肠癌(CRCs)是dMMR/MSI-H,而dMMR/MSI-H结肠癌患者更有可能是II期。显示dMMR/MSI-H状态的II期结肠癌患者并不能从5-FU单药的辅助化疗中获益。dMMR/MSI-H的II期CC患者伴有高危因素是否与预后有关尚不明确。辅助化疗在高危dMMR/MSI-H II期CC患者中的作用尚不明确。近期,Frontiers in Oncology杂志上发表了相关研究,旨在评估高危因素在dMMR/MSI-H II期CC的预后价值及其对辅助化疗的影响。
研究纳入2293例dMMR/MSI-H II期结肠癌(CC)患者。女性占58.2%;中位年龄为69岁(范围为21 - 90岁)。最常见的肿瘤部位为升结肠(32.5%),其次为盲肠(27.1%)和横结肠(13.1%)。乙状结肠和降结肠分别占9.7%和5.0%。在整个队列中,29.5% (n = 676)的患者被认为高危患者(≥1种高危因素)。切缘阳性、LVI和检查小于12个淋巴结患者比例分别为3.0、14.3和3.9%。14.0%的患者为pT4期。在高危患者中,36.1% (n = 244)接受辅助化疗,其中72.1% (n = 176)接受多药治疗,23.4% (n = 57)接受单药化疗,4.5% (n = 11)接受未知药物治疗。
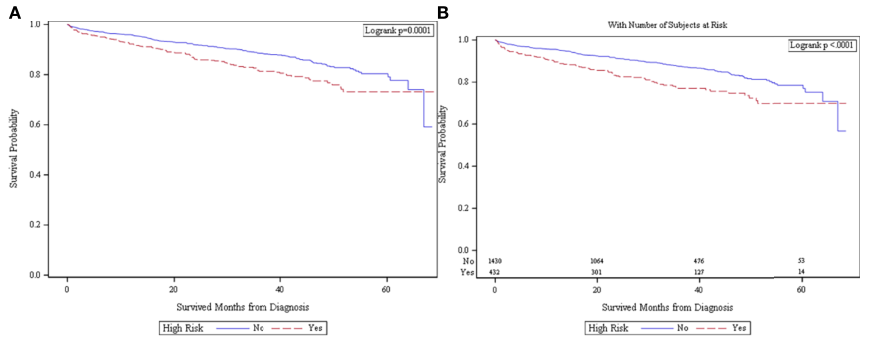
在整个队列中,当不按辅助化疗给药状态分层时,高危dMMR/MSI-H患者的OS较非高危dMMR/MSI-H患者更差[5年生存率和95%CI: 73.2% (67.3-78.1%) vs. 80.3% (76.7-83.5%), p = 0.0001]。在未接受辅助化疗的患者中,高危dMMR/MSI-H患者的OS较差[5年生存率和95%CI: 69.8% (62.6-75.9%) vs. 78.4% (74.3-81.9%), p<0.0001]。
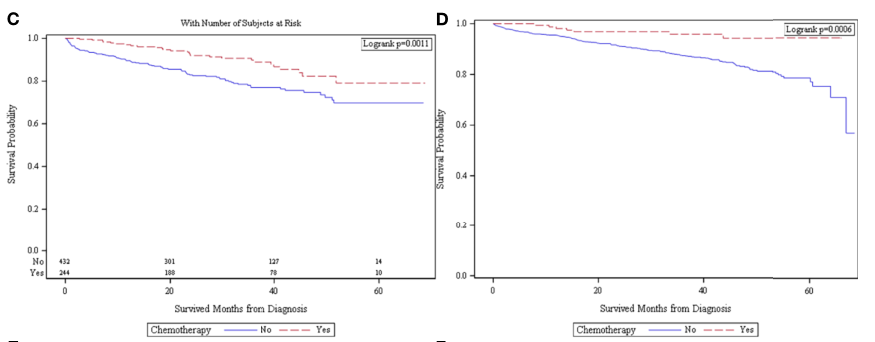
高危dMMR/MSI-H患者接受辅助化疗的OS优于未接受化疗的患者[5年生存率和95%CI: 78.0% (66.4-86.0%) vs. 69.8% (62.6-75.9%), p = 0.0011]。在无高危因素的患者中,接受辅助化疗的患者有更好的OS[5年生存率和95%CI: 94.3% (87.6-99.4%) vs. 78.4% (74.3-81.9%), p = 0.0006]。
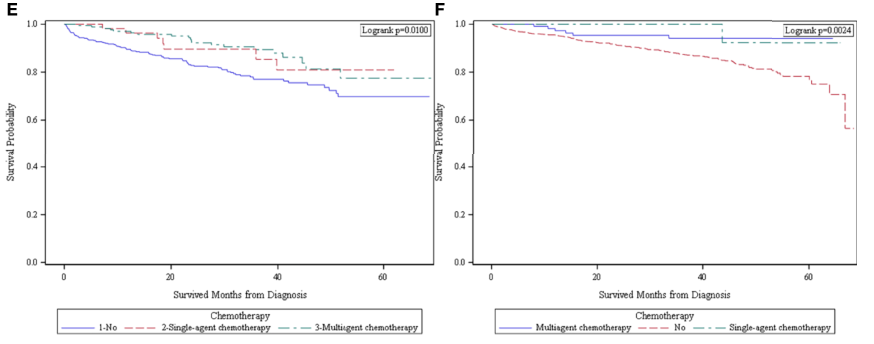
在单/多药辅助化疗患者组中,单药和多药化疗患者OS相似,均优于未化疗患者。这一发现在高危患者(p = 0.01)和无高危患者(p = 0.0024)中是一致的。
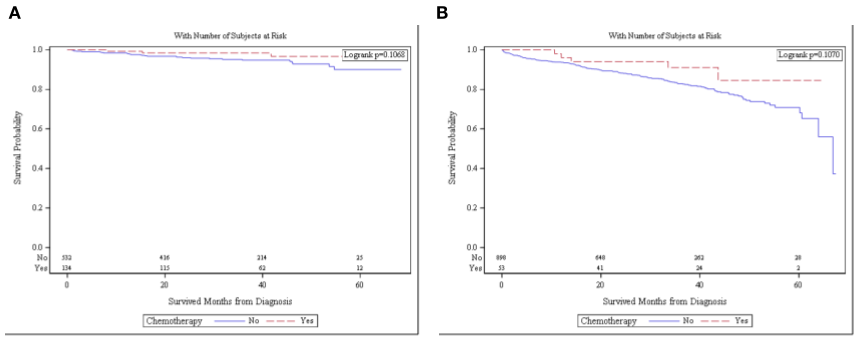
当无高危特征的患者按年龄分层时,化疗不再与更好的OS相关。无高危特征且年龄<65岁的患者接受化疗和不接受化疗的总生存期无差异[5年OS和95%CI: 96.7% (89.4-99.0%) vs. 90.0% (83.9-93.9%), p = 0.1068]。同一队列中≥65岁的患者接受化疗和不接受化疗的总生存率也没有统计学差异[5年生存率和95%CI: 96.1%(62.5-94.2%)和70.9% (65.1-75.9%),p = 0.1070]。
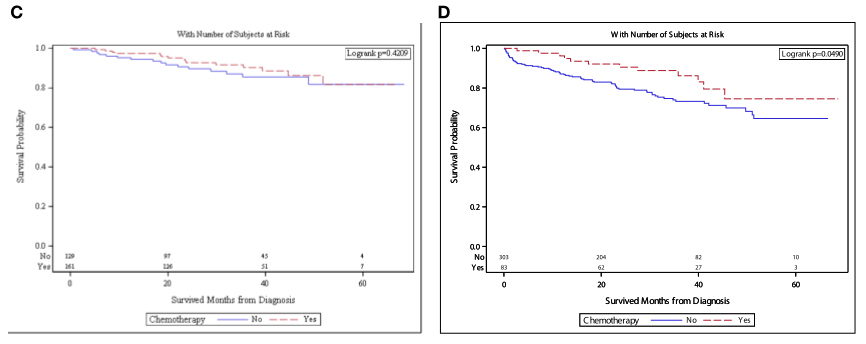
具有高危特征的患者的总生存率按年龄分层。<65岁患者中,接受化疗的患者与未接受化疗的患者的OS无差异[5年OS和95%CI: 81.7% (67.0-90.3%) vs. 81.8% (69.4-89.5%), p = 0.4209]。而≥65岁患者中,接受化疗患者的OS优于不接受化疗的患者[5年OS和95%CI: 74.5% (56.2-86.1%) vs 64.6% (55.5-72.3%),p = 0.0490]。
综上,研究表明,高危因素是dMMR/MSI-H II期结肠癌的预后因素。并且辅助化疗可以改善≥65岁高危dMMR/MSI-H II期结肠癌患者预后。
原始出处:
Mohamed A, Jiang R, Philip PA, Diab M, Behera M, Wu C, Alese O, Shaib WL, Gaines TM, Balch GG, El-Rayes BF and Akce M (2021) High- Risk Features Are Prognostic in dMMR/MSI-H Stage II Colon Cancer. Front. Oncol. 11:755113. doi: 10.3389/fonc.2021.755113
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
29
#dMMR/MSI-H#
47
#预后因素#
54
#MMR#
56
#MSI#
45
搜索不到原文啊
78