Cancer Immunol Immunother:DNA编码的抗前列腺特异膜抗原单克隆抗体的新的前列腺癌免疫疗法
2017-08-25 AlexYang MedSci原创
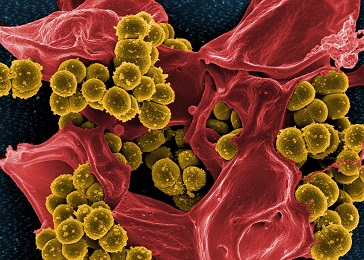
前列腺特异膜抗原(PSMA)在恶性肿瘤前列腺细胞中高水平表达,并且很可能是前列腺恶性肿瘤治疗的一个重要的药物靶标。目前已PSMA为治疗靶标的免疫疗法包括肽、细胞、载体或者基于DNA的疫苗以及PSMA特异性单克隆抗体(mAb)被动治疗。传统的mAb免疫治疗具有很多的逻辑和实践限制,包括高额的生产费用和由于短的mAb血清半衰期而导致的频繁剂量输入。最近,有研究人员阐释了一个基于抗体的免疫疗法的新的治疗
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#克隆#
34
#编码#
24
#抗原#
45
很好.不错.以后会多学习
88