胃切除术-正常解剖、手术适应症、手术切口、手术过程和手术预后(图片)
2015-12-03 网络 MedSci原创
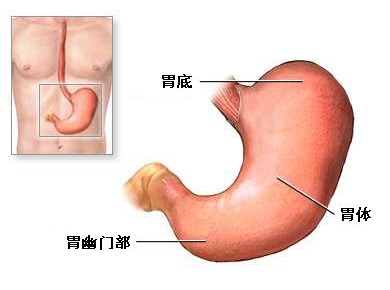
胃连接食管与小肠,其功能是把食物磨碎,以便小肠吸收营养物质。 慢性胃部疾病,如严重胃溃疡、胃癌,需要对胃部作部分或全切除。

胃连接食管与小肠,其功能是把食物磨碎,以便小肠吸收营养物质。

慢性胃部疾病,如严重胃溃疡、胃癌,需要对胃部作部分或全切除。

手术切口位于胃幽门部的体表投影。

术中切除有疾病的胃部分,小肠与残胃相连接,恢复消化道的通畅。

术后要对病人留置胃管减压,使胃保持空虚状态。数天后,当胃功能恢复,可以拔除胃管,给病人无渣流质饮食,逐渐过渡到正常饮食。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









简单易懂,科普文章
47
#切除术#
39
#手术切口#
38
#正常解剖#
40
简单表浅易懂
94
现在
87
好文章,值得收藏
85
说的也太简单了
141
#适应症#
24
#胃切除#
32