Diabetologia:20年研究发现,它能延长糖尿病患者寿命多达8年
2016-09-27 佚名 药明康德
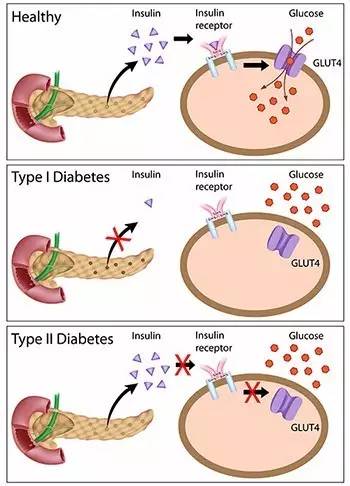
糖尿病患者,如何才能活得更久活得更好?近日,欧洲的科学家发现,专注于在早期对患者全方位强化管理,可使2型糖尿病中老年患者寿命延长8年之久,且在寿命延续期间也没有出现严重并发症。这将激发糖尿病研究领域转向于“老龄健康,延年益寿”策略。相关研究成果发布在欧洲糖尿病研究学会官方期刊《Diabetologia》上。糖尿病是由于人体内糖代谢紊乱而导致的一系列健康问题。它是一种慢性病,波及全球数亿人,而且发病

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#研究发现#
37
#DIA#
26
#BET#
24
总结经验非常好
55
总结的很好!
61
分享一下!
65
继续关注
52
继续学习
52
#糖尿病患者#
20
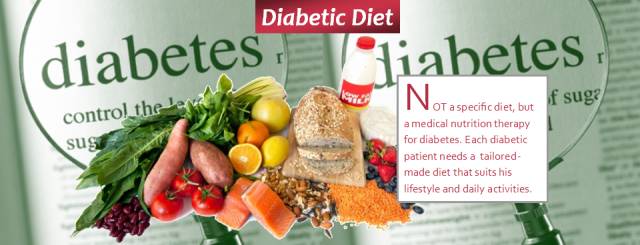
糖尿病要少食多餐
23