重复 NEJM:阿司匹林预防静脉血栓栓塞事件增添新证据
2018-03-03 杨中华 脑血管病及重症文献导读
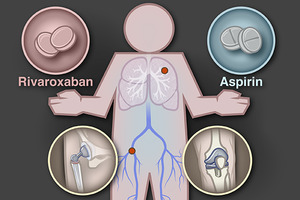
深静脉血栓形成(DVT)和肺栓塞(PE)通称为静脉血栓栓塞(VTE)是全髋或全膝关节成形手术的公认并发症。围手术期抗凝治疗被证明能够降低手术后VTE相关死亡和并发症。出院后延长时间预防也能获益,特别是全髋关节成形术的患者。对于全髋关节置换术或全膝关节置换术的患者,当前指南推荐预防性抗凝持续最少14天,建议应该预防持续到手术后35天。因为有效性、安全性和使用方便,直接口服抗凝剂常被用于长时间抗凝的选
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#栓塞事件#
32
#静脉血栓栓塞事件#
32
#静脉#
22
#静脉血#
34
学习了.谢谢分享
71
好
55