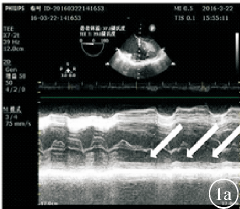
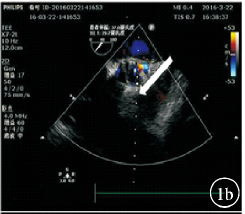
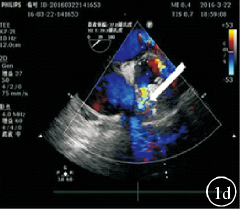
术中食道超声诊断右冠状动脉栓塞1例
2020-01-09 刘学兵 实用医院临床杂志
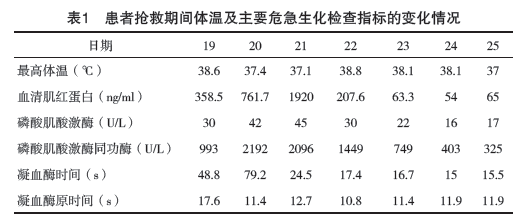
患者,女,43岁。因“主动脉瓣置换术后10年,发现再狭窄2天”于2016年3月22日入院。患者10年前因“先天性心脏病,主动脉瓣二叶畸形,主动脉瓣重度狭窄,左室肥厚”行主动脉瓣生物瓣置换术,手术过程顺利。2年前我院超声心动图随访示:主动脉瓣位人工生物瓣前向血流速度稍增快(AV=3.6m/s),主动脉瓣轻度狭窄,与4年前的检查无明显变化。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#冠状动脉栓塞#
40
#动脉栓塞#
26
#食道超声#
23
#超声诊断#
18
#超声诊断#
32