Eur Heart J:恩格列净治疗急性心肌梗死的效果分析
2022-08-31 MedSci原创 MedSci原创
在近期发生心肌梗死的患者中,恩格列净与26周内更显著的脑利钠肽前体N端水平降低相关,同时超声心动图功能和结构参数也显著改善。
钠-葡萄糖共转运体2抑制可降低有症状心衰患者因心衰住院和死亡的风险。然而,目前还缺乏研究这类药物在急性心肌梗死患者中的作用的试验。
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,在这项学术、多中心、双盲试验中,研究人员纳入了476例伴有肌酸激酶大幅升高(>800U/L)的急性心肌梗死患者。他们在经皮冠状动脉介入治疗72小时内每日一次随机分配10mg恩格列净或匹配的安慰剂治疗。
该研究的主要结局是26周后脑利钠肽前体N端的变化情况,次要结局包括超声心动图参数的变化。
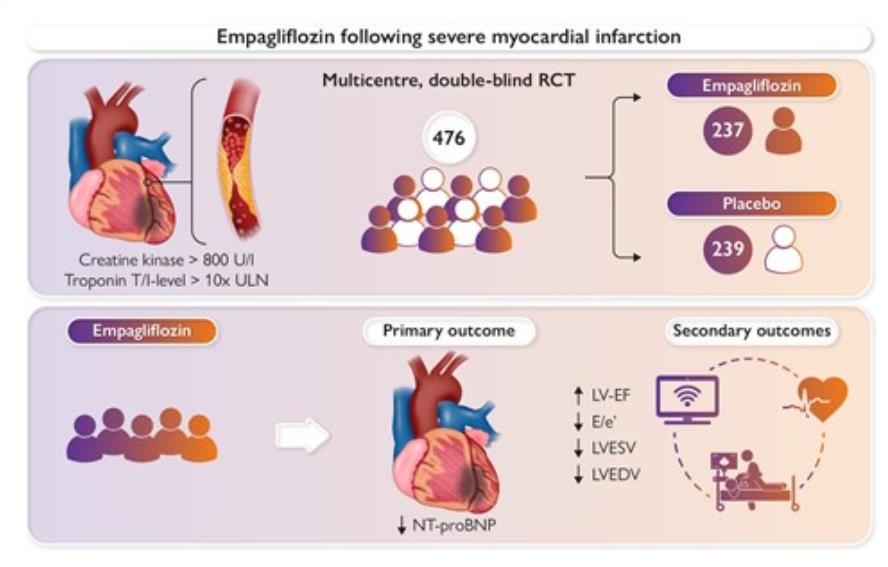
该研究的受试者基线脑利钠肽前体N端的中位数(四分位数范围)为1294(757-2246)pg/ml。经调整基线脑利钠肽前体N端、性别和糖尿病状态后,恩格列净组脑利钠肽前体N端的降低程度显著多于安慰剂组,降低了15%(95%可信区间[CI]为-4.4%至-23.6%)(p=0.026)。与安慰剂相比,恩格列净组绝对左室射血分数的改善程更加显著(1.5%,95%CI为0.2%-2.9%,p=0.029),平均E/E'降低6.8%(95%CI为1.3%-11.3%,p=0.015),左室收缩期末和舒张期末容积分别降低7.5ml(95%CI为3.4-11.5ml,p=0.0003)和9.7ml(95%CI为3.7-15.7ml,p=0.0015)。7例患者因心力衰竭住院(3例恩格列净组)。其他预先定义的严重不良事件很少见,组间没有显著差异。
由此可见,在近期发生心肌梗死的患者中,恩格列净与26周内更显著的脑利钠肽前体N端水平降低相关,同时超声心动图功能和结构参数也显著改善。
原始出处:
Dirk von Lewinski.et al.Empagliflozin in acute Myocardial Infarction: the EMMY trial.European Heart Journal.2022.https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehac494/6677315
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#效果分析#
41
#ART#
61
#HEART#
65