Kidney Int:肾脏纤维化发生机制研究获进展
2017-10-09 黄辛 中国科学报
复旦大学基础医学院陆利民课题组发现肾脏纤维化发生新机制,相关研究成果近日发表于《肾脏国际》杂志。
复旦大学基础医学院陆利民课题组发现肾脏纤维化发生新机制,相关研究成果近日发表于《肾脏国际》杂志。
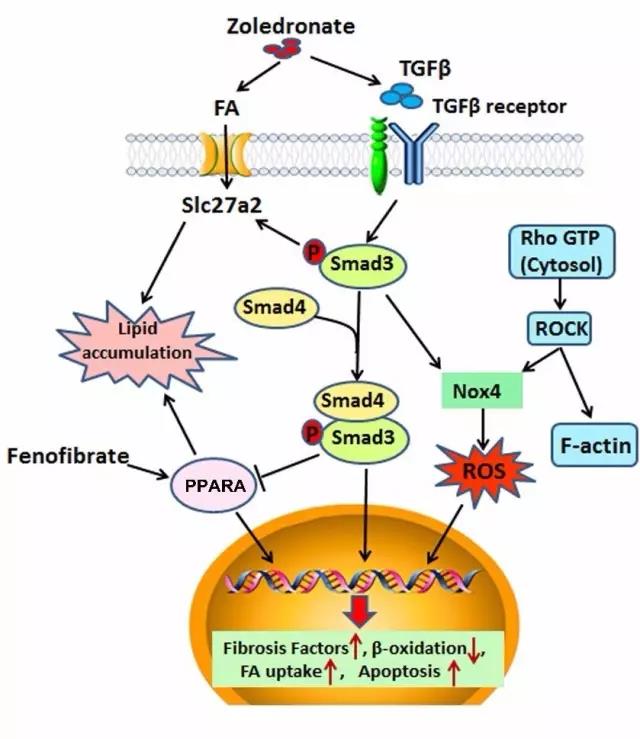
肾脏纤维化是各种原因造成肾脏损伤进入终末期的共同特征,而肾脏纤维化的进展速度决定了肾脏功能丧失的速度,延缓肾脏纤维化进展是保护肾脏功能的关键。病理情况下TGF-活化和过度生成在肾脏纤维化发生和发展中起关键作用,但调控TGF-活化的具体机制并不清楚。
C-Myc是重要的转录因子,也被誉为细胞重编程因子之一,参与细胞表型、功能、分化状态、细胞周期等的调控。陆利民课题组的研究成果证实,病理情况下肾脏组织中C-Myc异常升高,整合素V是直接受C-Myc调控的靶基因之一,通过促进整合素V的表达,C-Myc促使细胞外基质中处于潜伏状态的TGF-被释放、活化,促进肾脏间质细胞的活化,细胞外基质蛋白过度生成和沉积,继而促进肾脏纤维化发生和发展。
研究人员发现,在肾脏纤维化发生、发展过程中,肾脏小管上皮细胞、间质细胞、系膜细胞等多种肾脏固有细胞表型和功能发生了改变,而TGF-是调控上述改变的重要因子。
原始出处:
Yang Shen, Naijun Miao, Bao Wang,et al.c-Myc promotes renal fibrosis by inducing integrin αv-mediated transforming growth factor-β signaling.
Kidney International.October 2017Volume 92, Issue 4, Pages 888–899
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#研究获进展#
31
#机制研究#
29
#发生机制#
37
#kidney#
28