Blood:Suz12失活与JAK3突变信号协同促进T-ALL进展
2019-09-07 MedSci MedSci原创
PRC2复合物的核心成分是EZH2、SUZ12和EED,可促进组蛋白发生H3K27me3来使相关基因沉默。对419例T细胞急性淋巴细胞白血病(T-ALL)病例的测序数据的分析结果显示,SUZ12和JAK3突变之间具有显著的相关性。
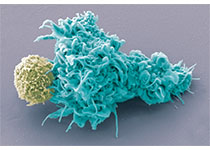
Suz12失活与JAK3突变信号协同驱动T-ALL的发展。
JAK3/Suz12突变白血病细胞对PI3K/mTOR、VEGFR和HSP90抑制剂的敏感性增强。
摘要:
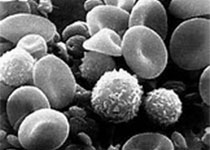
PRC2复合物的核心成分是EZH2、SUZ12和EED,可促进组蛋白发生H3K27me3来使相关基因沉默。对419例T细胞急性淋巴细胞白血病(T-ALL)病例的测序数据的分析结果显示,SUZ12和JAK3突变之间具有显著的相关性。
研究人员发现CRISPR/Case9介导失活Suz12协同JAK3突变可驱动T细胞转化和T-ALL进展。结合ChIP-seq和ATAC-seq数据的基因表达谱分析表明,Suz12失活导致PI3K/mTOR、VEGF和WNT信号增强。
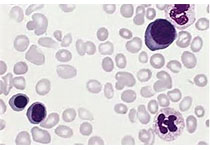
此外,药物筛选试验显示JAK3/Suz12突变型白血病细胞对HDAC6抑制的敏感性高于JAK3突变型白血病细胞。研究人员对Suz12失活后的全基因组表达变化进行综合分析发现,在JAK3和Suz12联合突变的T-ALL细胞中,PI3K/mTOR、VEGF/VEGFR和HDAC6/HSP90信号通路的易损性增加。
原始出处:
Michael Broux,et al.Suz12 inactivation cooperates with JAK3 mutant signaling in the development of T-cell acute lymphoblastic leukemia.Blood 2019 :blood.2019000015; doi: https://doi.org/10.1182/blood.2019000015
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JAK3#
37
#JAK#
32
#ALL#
20
#T-ALL#
26