TCT2015:高润霖院士报告ABSORB China研究
2015-10-21 CMT 中国医学论坛报
研究简介 当地时间10月12日上午,在美国经导管心血管治疗学(TCT)年会“最新揭晓临床试验”专场,中国医学科学院阜外医院高润霖院士报告了ABSORB China研究的主要结果。这项前瞻性、多中心、随机对照试验结果表明,依维莫司洗脱生物可吸收支架Absorb BVS在主要终点[一年血管造影随访病变节段内晚期管腔丢失(LL)]方面不劣于金属药物洗脱支架Xience CoCr-EES(钴
研究简介
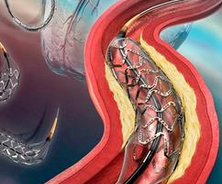
当地时间10月12日上午,在美国经导管心血管治疗学(TCT)年会“最新揭晓临床试验”专场,中国医学科学院阜外医院高润霖院士报告了ABSORB China研究的主要结果。这项前瞻性、多中心、随机对照试验结果表明,依维莫司洗脱生物可吸收支架Absorb BVS在主要终点[一年血管造影随访病变节段内晚期管腔丢失(LL)]方面不劣于金属药物洗脱支架Xience CoCr-EES(钴铬合金依维莫司洗脱支架)。文章同步发表于《美国心脏病学会杂志》(J Am Coll Cardiol)。
ABSORB China是全球第一个以常规一年血管造影随访病变节段内晚期管腔丢失为主要研究终点的临床研究,旨在评价Absorb BVS治疗冠脉狭窄病变的造影有效性及临床安全性和有效性,为Absorb BVS在中国获批上市提供依据。
该研究入选了中国24家中心、480例PCI患者,1:1随机分配接受BVS(n=241)或CoCr-EES(n=239)。在随访一年时,主要终点节段内LL在BVS组为0.19±0.38 mm(n=200),CoCr-EES组为0.13±0.38 mm(n=195),BVS达到了非劣效性终点(P非劣效=0.01)。此外,两组患者随访1年的靶病变失败率(由心源性死亡、靶血管心肌梗死或缺血驱动靶病变血运重建的复合终点)相似,BVS组和CoCr-EES组分别为3.4%、4.2%(P=0.62);两组明确/可能的支架血栓发生率也相似(0.4% 对0.0%,P=1.0)。
高院士总结说,“ABSORB China研究结果表明BVS在主要终点一年节段内晚期管腔丢失方面不劣于CoCr-EES,二者一年临床安全性和有效性相当,今后仍需要进一步研究评估BVS在复杂患者及复杂病变中的应用效果,并比较BVS与CoCr-EES的远期有效性及安全性。”
现场
专家点评
美国斯通(Gregg Stone)教授:我认为ABSORB China研究和ABSORB Japan研究都非常重要,经过严格的高比例1年造影随访,证实了BVS非常好的支架内皮覆盖和极小的晚期管腔丢失,与Xience支架相比仅增加0.05~0.1 mm,以及较低的、仅有个位数的再狭窄率。目前我们已经有了4个关于BVS与Xience支架对比的随机临床试验和数据,积累了很多应用BVS的经验。
正如我们今天上午讨论的,药物和器械的研究均在不断地进展但又有不同:替格瑞洛可能是主导今后20年的抗血小板药物;而介入器械每隔几年就会有所革新,新器械、新技术的出现又会引领临床预后的改善,介入术者必须要不断地跟上技术的革新步伐。我认为BVS的主要优势在于远期结果,因为支架的主体结构在3年内完全消失,没有异物遗留,这就带来很多长期的潜在优势,如没有涂层的反应、支架断裂、边支被封闭,或是金属负荷过重的风险。当然对于这些远期结果,我们还需要更长、特别是随访5年以上的临床研究来证实。
荷兰塞吕(Patrick Serruys)教授:给我印象最深的是0.23 mm的晚期管腔丢失,BVS在经历了不同的研究者、不同的核心实验室、不同的临床研究后,这个数字已经被证实是稳定的。由于BVS的支架丝较厚,所以为了达到内皮覆盖,晚期管腔丢失至少在150μm以上。如果我们能减小BVS支架丝的厚度,这个数值还可能会进一步改善,这一点可以通过今后的研究来证实。总体来看,这是一个非常好的研究结果。
荷兰米恩(Nicolas Mieghem)教授:我们以前关于BVS的经验都来自于欧洲的研究,其对BVS置入后的后扩张是有强制要求的,这一点与本研究中的要求不尽相同。介入术者开始应用BVS时,需要熟悉掌握BVS的特点和操作方法。
瑞士瓦尔吉米利(Marco Valgimigli)教授:不同研究的人群接受的治疗药物不同可能会对结果产生影响,在欧洲的研究人群中应用P2Y12受体拮抗剂更加积极,在美国人群中应用BVS时也要考虑这一点。此外,BVS的支架丝厚度对于晚期管腔丢失是一个重要的影响因素,我认为在今后的研究中应该将其作为重点进行改进。
加拿大乔利(Sanjit Jolly)教授:这项研究非常重要,对于这一临床试验结果,我们已经等了很长的时间,我们需要BVS在全球人群中应用的结果。现有的药物洗脱支架比如EES已经有很好的临床结果了,对于新的支架,我们需要证据来回答为什么我们需要更换为BVS,我想这需要更长时间的、更多的研究数据支持。
美国里昂(Martin Leon)教授:这是一项非常严谨的临床研究,达到了85%的造影随访率,我认为高院士及他的中国同事值得尊敬。就研究结果而言,我认为0.23 mm的晚期管腔丢失是很好的结果,这证实了BVS是完全可以与现有药物洗脱支架媲美的器械。但BVS与传统药物洗脱支架的操作技术有很大不同,远期的临床结果更是与操作方法有直接关系,所以对介入医生的要求更高,术者操作时需要更小心的预扩张与后扩张,仔细阅读影像,以得到最优的结果。
(现场专家点评由阜外医院宋雷、慕朝伟整理)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#高润霖#
47
#CHINA#
38
开
104
#TCT#
36
好复杂
101