重要的参数:动脉氧分压对比动脉血氧饱和度,作为重症监护氧合试验中的目标
2018-12-20 吴燕妮 重症医学
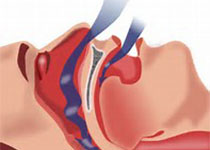
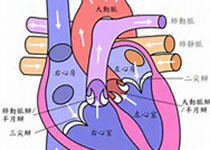
收入重症监护病房(ICU)的重症患者,尤其是有急性低氧性呼吸衰竭的患者的氧合目标,仍是一个有争论的话题。有越来越多的证据表明高氧有潜在的危害。然而,仍然不清楚最佳的氧合目标,在保证足够的氧合以避免低氧的伤害,同时尽量避免高氧。因此,需要对这一课题进行更大的随机临床试验。一些观察性研究以及干预前后的试验和3项小的随机对照试验为这一领域提供了有价值的,尽管不是决定性的证据。动脉氧饱和度(SaO2)或脉
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#动脉血#
40
#血氧饱和度#
39
#血氧#
0
#监护#
32
#氧饱和度#
33