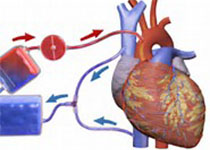
心肌缺血或可不做搭桥支架,专家解读无创新疗法
2017-05-08 陈明明 澎湃新闻
目前,我国心血管病患者约2.9亿,其中高血压2.7亿,脑卒中700万左右,心肌梗死250万左右。然而,搭桥、支架等等心脏介入治疗尽管挽救了一个又一个抢救患者的生命,却不能做到发病前的预防以及发病后的康复;大量发病后患者得不到进一步的医学指导,从而反复发病、反复住院……我国的心血管病治疗水平可能已达国际先进之列,但我国的心脏康复临床几乎处于空白阶段。中国科学院院士、中华医学会心血管病分会主任委员、上
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#专家解读#
31
#搭桥#
34
#创新#
29
#新疗法#
45
学习了
60
现在的患者大多数不重视康复这块。。就像扁鹊说的那样他们三兄弟,大哥医术最好一样。。防病于未然才是最好的。
49
谢谢分享,学习了!
72
又是一个技术的进步。
58
学习了,又提高了
61