PNAS:尤涵等解析神经母细胞瘤分化机制
2012-04-10 厦门大学生命科学学院 厦门大学生命科学学院
近日,国际权威学术期刊美国《国家科学院院刊》(PNAS)上发表了厦门大学生命科学学院的研究人员的研究论文,揭示了FOXO调控神经母细胞瘤分化的分子机制。 神经母细胞瘤(NB)是儿童常见的恶性肿瘤,年发病率大约为1/10万,仅低于白血病和中枢神经肿瘤。在神经母细胞瘤的发病过程中一个关键的早期事件就是成神经细胞不同阶段的分化停滞。利用TPA和PDGF-BB促使成神经瘤细胞终末分化可作为有效治疗神经细
近日,国际权威学术期刊美国《国家科学院院刊》(PNAS)上发表了厦门大学生命科学学院的研究人员的研究论文,揭示了FOXO调控神经母细胞瘤分化的分子机制。
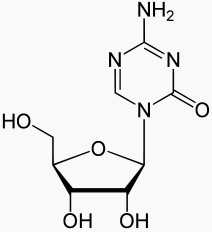
神经母细胞瘤(NB)是儿童常见的恶性肿瘤,年发病率大约为1/10万,仅低于白血病和中枢神经肿瘤。在神经母细胞瘤的发病过程中一个关键的早期事件就是成神经细胞不同阶段的分化停滞。利用TPA和PDGF-BB促使成神经瘤细胞终末分化可作为有效治疗神经细胞瘤的策略。然而直到现在研究人员对于这一过程中的信号通路还不是很清楚。
领导这一研究的是厦门大学生命科学学院教授、博士生导师尤涵。生命科学学院博士研究生梅杨,张蕾和第一医院王占祥为本文的共同第一作者。此项研究获得了科技部和国家自然科学基金委资助课题。
近年来,FOXO家族分子因在神经系统发育中的作用受到关注。已有研究表明:FOXO参与了神经干细胞(neural stem cell,NSCs)的稳态维持和分化;FOXO对神经元极化有至关重要的作用。PDGFRA属于受体酪氨酸激酶(Receptor Tyrosine Kinase,RTK)家族成员,研究表明其配体PDGF具有神经营养因子效应,可促进神经母细胞瘤细胞在应激条件下发生分化。
研究人员发现FOXO在生理条件和应激条件下(如血清饥饿)调控了PDGFRA的转录表达。在TPA诱导神经母细胞瘤细胞分化的研究体系中,他们进一步发现FOXO-PDGFRA通路对神经母细胞瘤细胞分化起决定性作用,并且阐明PDGFRA是FOXO调控神经母细胞瘤细胞分化的关键下游靶分子。
诱导神经母细胞瘤细胞分化是临床治疗神经母细胞瘤患者的手段之一,然而由于调控神经母细胞瘤分化的分子机理不甚明确,使得该治疗手段疗效甚微。
新研究结果揭示了TPA诱导NB分化的关键分子机制,为设计有效靶向药物逆转NB的分化提供了重要的理论依据。(生物谷Bioon.com)

doi:10.1073/pnas.1119535109
PMC:
PMID:
Regulation of neuroblastoma differentiation by forkhead transcription factors FOXO1/3/4 through the receptor tyrosine kinase PDGFRA
Mei, Yang; Wang, Zhanxiang; Zhang, Lei; Zhang, Yiru; Li, Xiaoyu; Liu, Huihui; Ye, Jing; You, Han
Neuroblastoma is a common childhood malignant tumor originated from the neural crest-derived sympathetic nervous system. A crucial early event in neuroblastoma pathogenesis is arrested differentiation of neuroblasts at various stages. Treatment of neuroblastoma with TPA and PDGF-BB leads to terminal differentiation of neuroblastoma cells. However, the signaling pathways that are involved in this process remain largely unknown. Here, we report that inhibition of endogenous FOXO proteins attenuated TPA/PDGF-BB mediated differentiation of neuroblastoma cells. Activated FOXO transcription factors acted on PDGFRA promoter to direct its basal mRNA expression as well as its induction upon serum deprivation. Depletion of endogenous PDGFRA in neuroblastoma cells significantly diminished neurite formation and extension under TPA/PDGF-BB treatment. Furthermore, ectopic expression of PDGFRA abolished the blockage of neuroblastoma differentiation by FOXOs inhibition. These findings define the FOXO–PDGFRA axis as crucial mechanistic components that govern TPA-induced neuroblastoma differentiation.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#母细胞瘤#
30
#分化机制#
45
#解析#
40
#PNAS#
39
#细胞瘤#
41