Oncotarget:几种重要的免疫因子和原发性肉瘤临床之间亚型相关
2017-07-21 Emma MedSci原创
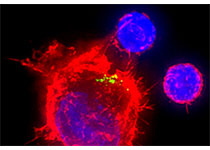
肉瘤属于恶性肿瘤病变,是来源于间叶组织的恶性肿瘤,多发生于皮下、皮肤、骨膜及长骨两端。骨肉瘤多发于青壮年,发展迅速且病程短。为了探究肉瘤的免疫检查点阻滞潜力,发表于Oncotarget的一篇文章中,研究人员调查了208例肉瘤患者肿瘤中程序性细胞死亡分子-1(PD-1),程序性死亡配体-1(PD-L1)、CD8的表达和临床的相关性。结果显示,PD-1、PD-L1和CD8的表达和临床之间是亚型相关的。
肉瘤属于恶性肿瘤病变,是来源于间叶组织的恶性肿瘤,多发生于皮下、皮肤、骨膜及长骨两端。骨肉瘤多发于青壮年,发展迅速且病程短。为了探究肉瘤的免疫检查点阻滞潜力,发表于Oncotarget的一篇文章中,研究人员调查了208例肉瘤患者肿瘤中程序性细胞死亡分子-1(PD-1),程序性死亡配体-1(PD-L1)、CD8的表达和临床的相关性。结果显示,PD-1、PD-L1和CD8的表达和临床之间是亚型相关的。
免疫组化检查原发性未经治疗的骨肉瘤(n = 46),尤文肉瘤(n = 32),腺泡型横纹肌肉瘤(n=20),胚胎型横纹肌肉瘤(n = 77),滑膜肉瘤(n = 22)和促结缔组织增生性小圆细胞肿瘤(DSRCT)(n = 11)。PD-L1的表达主要在腺泡型横纹肌肉瘤和胚胎型横纹肌肉瘤中检测到(分别为15%和16%);在腺泡型横纹肌肉瘤中,PD-L1表达与更好的总体生存期、无疾病生存期和无转移生存期相关。PD-1在淋巴细胞上的表达主要见于滑膜肉瘤(18%)。高水平的CD8 +淋巴细胞主要在骨肉瘤中检出(35%),并且与滑膜肉瘤的无疾病生存期差有关。此外,在尤文肉瘤和DSRCT中,检出PD-1在肿瘤细胞上,而不是肿瘤浸润淋巴细胞,这是相关研究中研究人员首次报道PD-1在尤文肉瘤(19%)和DSRCT(82%)肿瘤细胞上的表达。
原始出处:
van Erp AEM, et al. Expression and clinical association of programmed cell death-1, programmed death-ligand-1 and CD8+ lymphocytes in primary sarcomas is subtype dependent. Oncotarget. 2017 Jul 7. doi: 10.18632/oncotarget.19071.
本文系梅斯医学(MedSci)原创翻译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#免疫因子#
28
#原发性肉瘤#
51
#target#
31
#原发性#
26
内容很好多谢分享
66
.内容很好,学习了.
50
好好学习学习学习
67
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。给点赞啦
59
开拓了思路
47
谢谢分享,学习了!
30