JACC:CTA联合 CTP用于动态心肌灌注成像能显著提高诊断性能
2021-11-15 MedSci原创 MedSci原创
与单独的CTA相比,将冠状动脉CTA的解剖学评估和动态CTP的功能评估相结合,可以更准确地识别具有血流动力学意义的CAD。
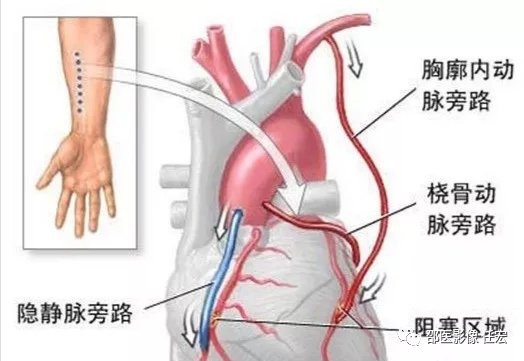
心脏冠状动脉血管成像(CTA)目前被广泛应用于冠心病的诊断、无症状冠心病的筛查、先天性冠状动脉异常诊断、冠脉支架植入术后随访等情况,是诊断冠状动脉疾病的主要无创影像学工具,且已成为实施经导管冠状动脉造影和经皮冠状动脉介入治疗的“看门人”,对有胸痛症状、疑诊冠心病的患者有重要的诊断价值。
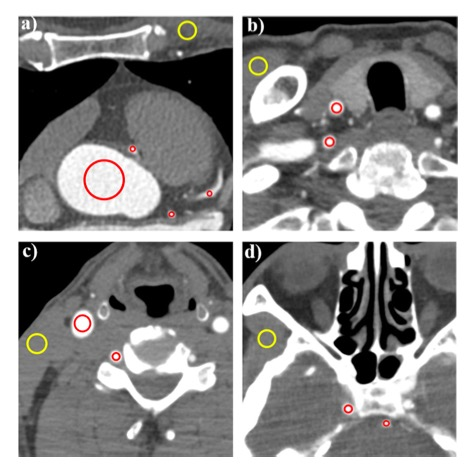
计算机断层扫描灌注(CTP)是评估急性缺血性卒中的有用工具,它可以提供缺血核心和缺血性半影的估计。单中心研究表明,动态CTP成像在诊断冠状动脉疾病(CAD)方面具有很高的诊断准确性。
为了确定了联合冠状动脉计算机断层扫描(CTA)和CTP在检测由有创冠状动脉造影(ICA)定义的具有血流动力学意义的CAD时的诊断性能。来自日本的科学家开展了一项前瞻性的多中心研究,结果发表在JACC杂志上。

研究人员在七个中心招募了174名疑似或已知的CAD患者,他们在临床上被转诊为ICA。在ICA前使用双源CT进行CTA和动态CTP。在冠状动脉直径狭窄26%至90%的情况下,FFR作为ICA的一部分进行。血流动力学意义上的狭窄被定义为FFR<0.8或ICA上>90%的狭窄。
最终157名参与者完成了研究方案,157名患者中的76名(48%)和442条血管中的112条(25%)检测到血流动力学上的显著狭窄。根据接受者操作特征曲线(AUC)分析,在CTA中加入动态CTP,在患者层面上,曲线下面积从0.65(95%CI:0.57-0.72)明显增加到0.74(95%CI:0.66-0.81;P=0.011),敏感性下降(93% vs 72%;P<0.001),特异性提高(36% vs 75%;P<0.001),总体准确性提高(64% vs 74%;P<0.001)。
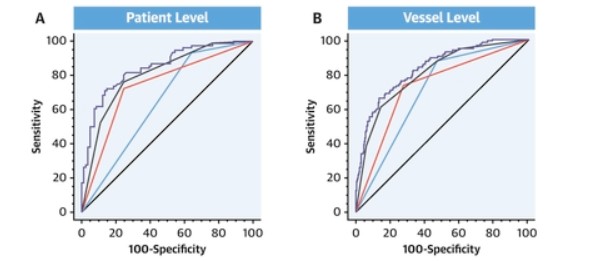
使用CTA+CTP在诊断CAD中的ROC曲线
在这项关于动态CTP的前瞻性多中心研究中,与单独的CTA相比,将冠状动脉CTA的解剖学评估和动态CTP的功能评估相结合,可以更准确地识别具有血流动力学意义的CAD。然而,这种方法的临床意义还需要进一步研究,包括其对改善预后的作用。
参考文献:
Diagnostic Performance of Dynamic Myocardial Perfusion Imaging Using Dual-Source Computed Tomography. J Am Coll Cardiol. 2021 Nov, 78 (20) 1937–1949
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#JACC#
51
#诊断性#
46
#灌注成像#
52
#心肌灌注#
66
#CTA#
42
#CTP#
49
#ACC#
39
通气患者的一个重要问题,其危险因
67