JACC:ACC前主席痛批“易损斑块”理念!脂质斑块与远期事件无关
2020-04-17 xujing 文韬 中国循环杂志
富含脂质的斑块属于高危斑块。对于脂质斑块罪犯病变的介入治疗,一些病理学研究提示会出现远端栓塞和损伤部位愈合而恶化预后。
富含脂质的斑块属于高危斑块。对于脂质斑块罪犯病变的介入治疗,一些病理学研究提示会出现远端栓塞和损伤部位愈合而恶化预后。
近期,JACC发表的一项前瞻注册研究有两个重要发现,一是脂质斑块与远期事件不相关。二是介入治疗富含脂质斑块病变是安全的,不影响介入治疗短期或2年预后。
而且,在接受介入治疗的1621例患者中,2年随访时,有高达18%的患者发生了不良心血管事件。
但只有8.3%的事件与罪犯血管(即接受治疗的血管)有关,10.7%的事件与其他血管有关。
研究纳入1999例患者,平均年龄64岁,77.9%为男性,39.4%为糖尿病患者。
研究发现,罪犯血管发生不良心血管事件的患者更年轻,有更多的糖尿病和冠状动脉再血管化史,特别是旁路手术史。病变也更复杂、更长、最终支架内最小管腔直径更小和更少使用药物洗脱支架。使用二代药物支架者发生事件者较少。
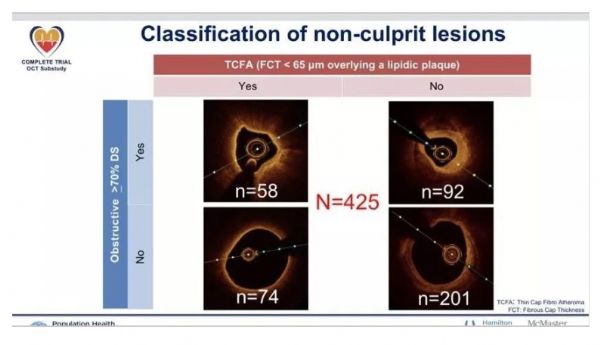
该研究中,共有1189例患者在PCI术前接受了1283个病灶的红外光谱显像检查。
9例患者出现红外光谱显像相关并发症,其中1例发生围手术期心肌梗死,1例需要紧急搭桥手术。
研究者对接受红外光谱显像检查的患者进行了分析,发现在任何4 mm长的病变血管内,罪犯病变相关2年心血管事件发生率与最大脂质核心负荷指数没有显著相关性。
在同期述评中,ACC前主席Steven Nissen教授指出,在许多情况下,一些医生希望识别易损斑块,并植入支架,以避免不良后果。而甚至有医生测量了斑块温度,然后将支架置入无明显狭窄的部位,以“预防”未来的冠脉事件。
而且,在这一理论的驱动下,易损斑块检测技术层出不穷:热成像、血管内超声(IVUS)虚拟组织学、光学相干断层扫描称、血管镜、血管内磁共振、近红外光谱(NIRS),血管内弹性成像、多探测器计算机断层扫描和正电子发射断层扫描。但这些方法均未通过精心设计的随机对照研究得到验证,也没有常规临床应用。
众多研究发现,似乎非常清楚的是,易损斑块的整个概念从根本上来说是有缺陷的,反映了对冠状动脉事件的病理生理学的过于简单的认识。
Nissen教授指出,发表的这项研究的设计和实施存在重大缺陷。介入医生对斑块的影像学结果很清楚,而且可以随意更决定介入治疗。
他认为,我们现在主要问题是将注意力仅仅集中在单个斑块上。尽管多数冠脉事件确实发生在某个部位,但动脉粥样硬化是系统性疾病,而非局灶性病变。有研究发现,几乎所有冠脉部位都存在一定程度的斑块。
治疗单一易损斑块的概念过于简单。治疗应基于疾病的病理生理学特征,缺血事件的发生是由炎症、高水平C-反应蛋白和血小板反应性等系统性因素驱动,而不是斑块的形态。已证明可减少冠脉事件的方法,都是全身性疗法,例如降脂、抗血小板药物和抗炎等。
Nissen认为,经过成千上万的易损斑块研究,针对单一易损斑块的努力可以休矣。
原始来源:
Myong Hwa Yamamoto, et al. 2-Year Outcomes After Stenting of Lipid-Rich and Nonrich Coronary Plaques. J Am Coll Cardiol. 2020, 75 (12) 1371-1382.
Steven E. Nissen. Vulnerable Plaque and Einstein’s Definition of Insanity. J Am Coll Cardiol. 2020, 75 (12): 1383-1385.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#JACC#
28
#ACC#
37
#斑块#
25
#脂质斑块#
37