Nature Nanotechnol:肿瘤血管正常化有助化疗药物递送
2012-04-16 Beyond 生物谷
旨在提高癌症治疗的结果的抗血管生成药物和纳米药物两种治疗策略的结合只有当使用最小纳米药物的时候,这两种治疗策略的结合才可能是成功的。美国马萨诸塞州总医院(MGH)研究人员在《自然纳米技术》上发表文章称:肿瘤组织内血管正常化能提高标准化疗药物的传递,可以阻止更大的纳米药物分子进入肿瘤血管。 麻省总医院放射肿瘤科斯蒂尔肿瘤生物学实验室Vikash P. Chauhan说:我们发现血管正常化不仅促
旨在提高癌症治疗的结果的抗血管生成药物和纳米药物两种治疗策略的结合只有当使用最小纳米药物的时候,这两种治疗策略的结合才可能是成功的。美国马萨诸塞州总医院(MGH)研究人员在《自然纳米技术》上发表文章称:肿瘤组织内血管正常化能提高标准化疗药物的传递,可以阻止更大的纳米药物分子进入肿瘤血管。
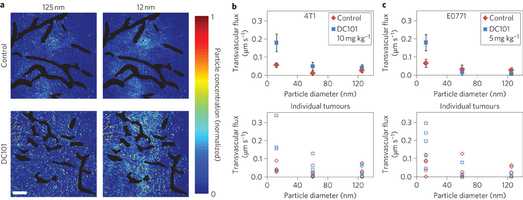
麻省总医院放射肿瘤科斯蒂尔肿瘤生物学实验室Vikash P. Chauhan说:我们发现血管正常化不仅促进了最小的纳米药物进入癌细胞,我们还发现最小的纳米药物天生就比大的纳米药物能更容易穿透肿瘤组织,这表明小的纳米药物可能是治疗癌症的理想选择。
肿瘤需要生成自己血管以供应能量,但肿瘤血管往往杂乱无章。肿瘤血管不仅防止了化疗药物传递到细胞无法靠近肿瘤血管,并且血管的血浆渗漏性增加肿瘤内的压力能进一步减少药物渗透到肿瘤组织能的能力。通过抑制血管生成药物的治疗可以减少这些异常,这一过程被称为血管正常化,其与标准化疗药物联合运用已被证明可以改善某些癌症的治疗。
纳米药物实际上是依据利用肿瘤血管异常设计的。标准化疗药物的分子约一纳米,纳米分子从10到100倍大,不足以穿透正常组织的血管毛孔,但却能通过超大的毛孔传递倒肿瘤血管中。
麻省总医院团队编写了一个数学模型预测,肿瘤血管壁异常大的毛孔导致肿瘤内压力增加,阻碍药物进入肿瘤内,抗血管生成治疗减少毛孔孔径减少瘤内压力,使得这些药物分子通过大小合适的毛孔进入肿瘤血管。
美国哈佛大学工程与应用科学专业学生Chauhan说:目前在临床试验中使用或多种抗癌纳米药物,我们的研究结果表明小的纳米药物结合抗血管生成疗法可能有协同效应。斯蒂尔实验室主任Rakesh K. Jain博士表示:我们的研究提供指引上如何结合纳米药物与抗血管生成药物。(生物谷:Bioon.com)

doi:10.1038/nnano.2012.45
PMC:
PMID:
Normalization of tumour blood vessels improves the delivery of nanomedicines in a size-dependent manner
Vikash P. Chauhan,Triantafyllos Stylianopoulos,John D. Martin,Zoran Popovi,Ou Chen,Walid S. Kamoun,Moungi G. Bawendi,Dai Fukumura& Rakesh K. Jain
The blood vessels of cancerous tumours are leaky1, 2, 3 and poorly organized4, 5, 6, 7. This can increase the interstitial fluid pressure inside tumours and reduce blood supply to them, which impairs drug delivery8, 9. Anti-angiogenic therapies—which ‘normalize’ the abnormal blood vessels in tumours by making them less leaky—have been shown to improve the delivery and effectiveness of chemotherapeutics with low molecular weights10, but it remains unclear whether normalizing tumour vessels can improve the delivery of nanomedicines. Here, we show that repairing the abnormal vessels in mammary tumours, by blocking vascular endothelial growth factor receptor-2, improves the delivery of smaller nanoparticles (diameter, 12 nm) while hindering the delivery of larger nanoparticles (diameter, 125 nm). Using a mathematical model, we show that reducing the sizes of pores in the walls of vessels through normalization decreases the interstitial fluid pressure in tumours, thus allowing small nanoparticles to enter them more rapidly. However, increased steric and hydrodynamic hindrances, also associated with smaller pores, make it more difficult for large nanoparticles to enter tumours. Our results further suggest that smaller (~12 nm) nanomedicines are ideal for cancer therapy due to their superior tumour penetration.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
34
#肿瘤血管#
29
#TEC#
35
#化疗药物#
35
#化疗药#
36