Cancer Cell:同一种儿童脑瘤为何预后不同?
2016-04-08 佚名 生物谷
本文亮点: WNT-成神经管细胞瘤缺少血脑屏障,而该疾病的其他亚型不存在这种情况 WNT-成神经管细胞瘤能够分泌WNT拮抗物阻止血脑屏障形成 血脑屏障的功能决定了不同成神经管细胞瘤亚型对化疗药物暴露和应答的情况 可以通过改变成神经管细胞瘤的血管信号影响血脑屏障 近日,来自英国剑桥大学的科学家们发现不同亚型的成神经管细胞瘤在血脑屏障的功能方面存在差别,而这种差别可能是导致不同亚型预后
本文亮点:
WNT-成神经管细胞瘤缺少血脑屏障,而该疾病的其他亚型不存在这种情况
WNT-成神经管细胞瘤能够分泌WNT拮抗物阻止血脑屏障形成
血脑屏障的功能决定了不同成神经管细胞瘤亚型对化疗药物暴露和应答的情况
可以通过改变成神经管细胞瘤的血管信号影响血脑屏障

近日,来自英国剑桥大学的科学家们发现不同亚型的成神经管细胞瘤在血脑屏障的功能方面存在差别,而这种差别可能是导致不同亚型预后不同的重要原因。相关研究结果发表在国际学术期刊Cancer Cell上。
成神经管细胞瘤是比较常见的儿童颅内恶性肿瘤,根据分子分型不同,成神经管细胞瘤可以分为四种不同的亚型,而不同亚型的预后存在很大差别,其中WNT-成神经管细胞瘤是一种可治愈的亚型,而SHH-成神经管细胞瘤亚型则很难治愈,为何出现这种治疗效果的差别一直没有得到深入研究。
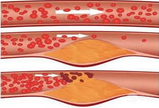
在这项研究中,研究人员发现在WNT-成神经管细胞瘤中突变的β-catenin驱动产生旁分泌信号,能够诱导出现异常的血管穿孔,这种现象反而能够使化疗药物在肿瘤内部高度积累,导致肿瘤产生强力治疗应答。
与之相比,SHH-成神经管细胞瘤存在着完整的血脑屏障,因此化疗药物很难渗透到肿瘤内部,导致出现肿瘤对药物的抵抗。该研究表明,在体内条件下调节成神经管细胞瘤-内皮细胞旁分泌轴有助于改变化疗药物的渗透性以及临床应答。
综上所述,成神经管细胞瘤的不同分型决定了肿瘤血管的表型,这部分解释了不同成神经管细胞瘤亚型之间迥然不同的预后,同时也为增强其他脑部肿瘤的化疗应答性找到了新的途径。
原始出处:
Timothy N. Phoenix, et al.Medulloblastoma Genotype Dictates Blood Brain Barrier Phenotype.Cancer cell.31 March 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
31
#Cell#
33
#cancer cell#
32
高大上的文章
122
ds值得关注
126
#脑瘤#
27
分型。。。
149
血药浓度
95