Lancet Oncol:EGFR/ALK阳性的NSCLC多线靶向治疗后仍可用免疫治疗?
2018-03-20 佚名 肿瘤资讯
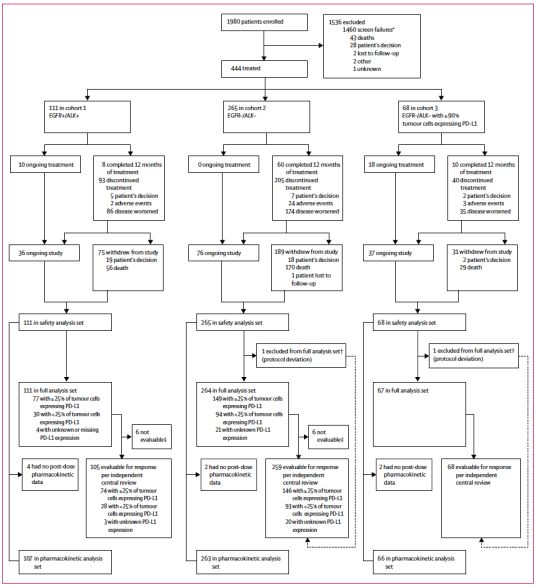
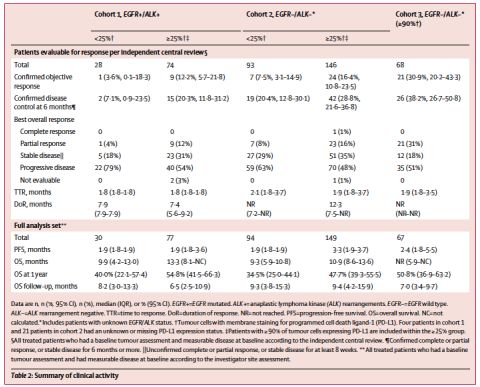
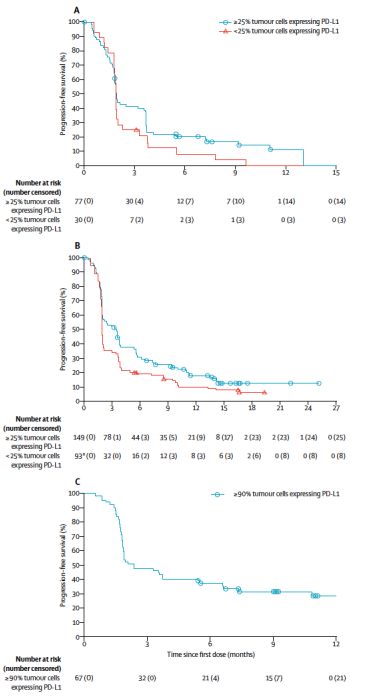
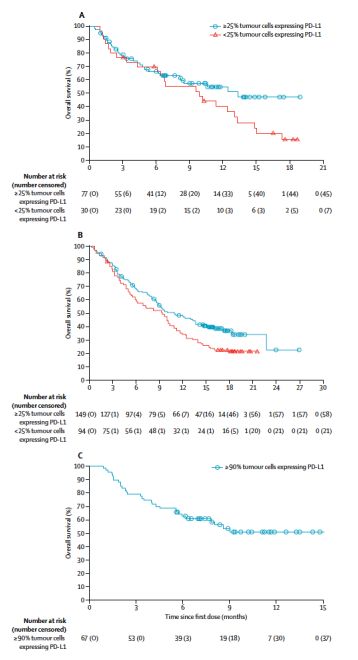
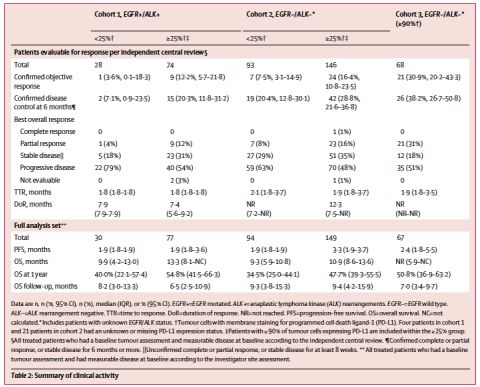
抗PD-L1单抗durvalumab目前已经获批用于接受了同步放化疗后未进展的局部晚期NSCLC的维持治疗。近日,durvalumab用于晚期NSCLC三线或以上治疗的II期临床试验ATLANTIC研究结果在《Lancet Oncology》杂志发表。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ALK阳性#
45
#Oncol#
24
#Lancet#
36
学习了很有用不错
60
#GFR#
28
学习
58
学习了.很好
60