JCC: 粪便微生物移植在维持溃疡性结肠炎患者缓解中的作用
2019-10-03 不详 MedSci原创
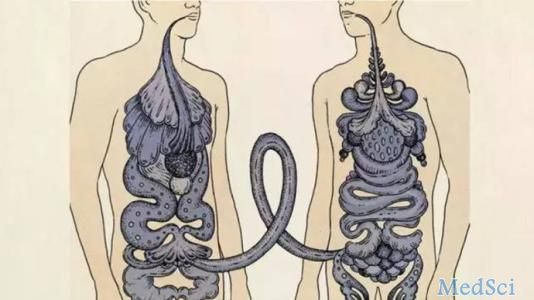
本项研究旨在探究粪便菌群移植[FMT]在维持溃疡性结肠炎[UC]缓解中的作用。
目标
方法
在这项前瞻性研究中,多疗程FMT后达到UC临床缓解的UC患者每8周随机分配一次维持FMT或安慰剂结肠镜检查输注,持续48周。所有患者均继续接受标准护理[SOC]治疗。主要观察终点是在第48周维持无类固醇的临床缓解[Mayo评分≤2,所有子评分≤1]。次要终点是在60天内达到内窥镜缓解[内镜Mayo评分0]和第48周时的组织学缓解[Nancy等级0、1]。
结果
共有61例临床缓解的患者被随机分配接受FMT [ n = 31]或安慰剂[ n = 30]。分配FMT的27/31 [87.1%]患者与使用安慰剂的20/30 [66.7%]患者[ p = 0.111] 达到临床缓解。内窥镜缓解的次要终点(FMT:18/31 [58.1%] vs安慰剂:8/30 [26.7%],p = 0.026)和组织学缓解(FMT:14/31 [45.2%] vs安慰剂:5/30 [ 16.7%],p= 0. 033)的FMT患者人数明显增加。没有严重的不良事件导致必须停止FMT的患者。
结论
本项研究表明处于临床缓解期的患者使用FMT维持治疗可以有助于维持UC患者的临床,内镜和组织学缓解。
原始出处:
Ajit Sood. Et al. Role of Faecal Microbiota Transplantation for Maintenance of Remission in Patients With Ulcerative Colitis: A Pilot Study. Journal of Crohn's and Colitis.2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#溃疡性#
38
#粪便微生物#
37
#微生物#
36
#粪便#
42