ERJ:肺血管阻力可预测与间质性肺病相关的肺动脉高压患者的死亡率-COMPERA 注册的结果
2021-10-13 刘少飞 MedSci原创
肺动脉高压(PH)是许多慢性肺部疾病的常见并发症,尤其是COPD和间质性肺病(ILD)。 在这些情况下,PH 的发展与症状的加重和死亡风险的增加有关。 在大多数慢性肺病患者中,PH 的血流动力学严重程

肺动脉高压(PH)是许多慢性肺部疾病的常见并发症,尤其是COPD和间质性肺病(ILD)。 在这些情况下,PH 的发展与症状的加重和死亡风险的增加有关。 在大多数慢性肺病患者中,PH 的血流动力学严重程度为轻度至中度,而一些患者会发展为重度 PH,目前定义为平均肺动脉压 (mPAP) ⩾ 35 mmHg 或 mPAP ⩾ 25 mmHg。 心脏指数 <2.0 L·min−1·m−2。 这些血流动力学标准是根据专家共识引入的,但并非基于可靠数据。
在与COPD相关的PH患者中,ZEDER 等人最近表明,肺血管阻力 (PVR)>5WU 是死亡率的最强血流动力学预测指标,作者建议使用该阈值来定义这组患者的严重 PH。 我们想知道这个阈值是否也适用于患有与 ILD 相关的 PH (PH-ILD) 的患者。
为了解决这个问题,我们分析了来自肺动脉高压新开始治疗的比较前瞻性登记处 (COMPERA) 的数据。 简而言之,COMPERA 是一个大规模的基于网络的 PH 登记处,它前瞻性地收集有关接受 PH 治疗的患者的特征、治疗和结果的详细数据。 来自欧洲各国(奥地利、比利时、德国、希腊、匈牙利、意大利、拉脱维亚、立陶宛、荷兰、斯洛伐克、瑞士和英国)的PH中心参与其中,约80%的入组患者来自德国。
COMPERA入选患者:
1) 2006 年 6 月 13 日至 2021 年 1 月 21 日期间新诊断为 PH-ILD 的成年患者;
2) 包含 mPAP ⩾ 25 mmHg 和肺动脉楔压 (PAWP) ⩽15 mmHg 时可用的血液动力学;
3) 至少一次记录在案的随访。 连续数据以中位数和第一和第三四分位数(Q1、Q3)表示,分类数据以数量和百分比表示。随访于 2021年4月30日结束。
在截止日(2021 年 5 月 1 日),COMPERA 数据库中登记了 10651 名患者,其中 662 名患者被归类为 PH-ILD。 其中,213 名患者因以下原因被排除:基线访视前 6 个月以上的 PH 诊断(n=73),年龄 <18 岁(n=2),任何时间进行肺移植 (n=29),没有记录的随访 (n=55),未能满足血液动力学纳入标准(无基线 PVR 值,n=50;PAWP >15 mmHg 或 mPAP <25 mmHg,n=61)。 最后,449 名患者符合本分析的条件。
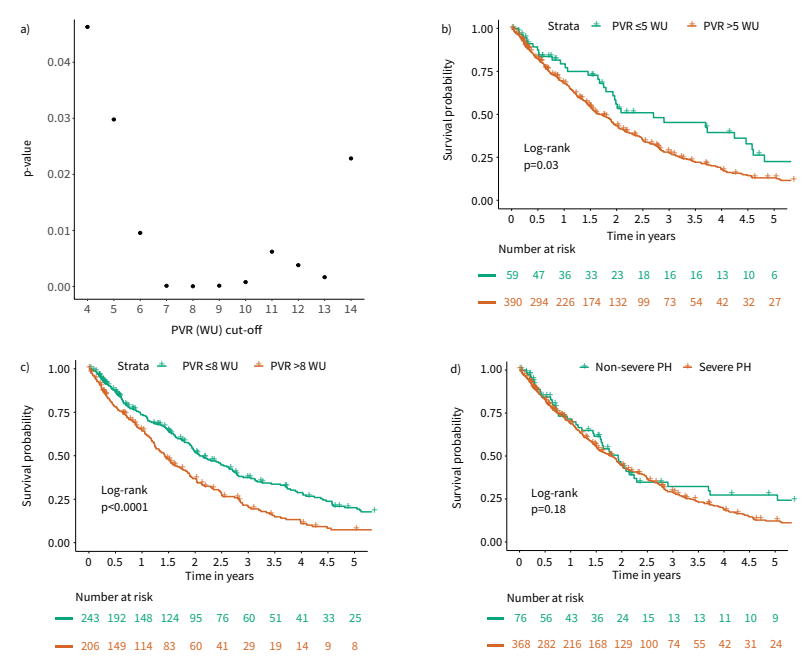
对 PH-COPD 患者的分析,PVR > 5 WU 是最好的预后截止值,而在我们对 PVR-ILD 患者的分析中,在 PVR 处看到了幸存者和非幸存者之间的最佳区分 >8 WU。 然而,我们的分析还表明,随着 PVR > 5 WU,死亡率显着增加。 同时,在本分析中未发现当前基于 mPAP 的慢性肺病严重 PH 定义具有预后意义。 基于这些发现,同时考虑到本次分析和之前分析的局限性,我们认为 PVR > 5 WU 应该用于定义慢性肺病患者是否存在严重 PH。
文章出处:
Olsson KM, Hoeper MM, Pausch C, Grünig E, Huscher D, Pittrow D, Rosenkranz S, Gall H. Pulmonary vascular resistance predicts mortality in patients with pulmonary hypertension associated with interstitial lung disease: results from the COMPERA registry. Eur Respir J. 2021 Aug 26;58(2):2101483. doi: 10.1183/13993003.01483-2021. PMID: 34385266.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#间质性#
46
#MPE#
35
#肺动脉高压患者#
45
#PE#
22
#肺病#
31
#动脉高压#
28
#肺血管阻力#
36
#ERA#
22
#注册#
38