精彩推荐:冠状动脉系统解剖、CTA解剖、分段及中英文名称对照
2023-03-04 华夏影像诊断中心 华夏影像诊断中心 发表于安徽省
冠状动脉系统解剖、CTA解剖、分段及中英文名称对照
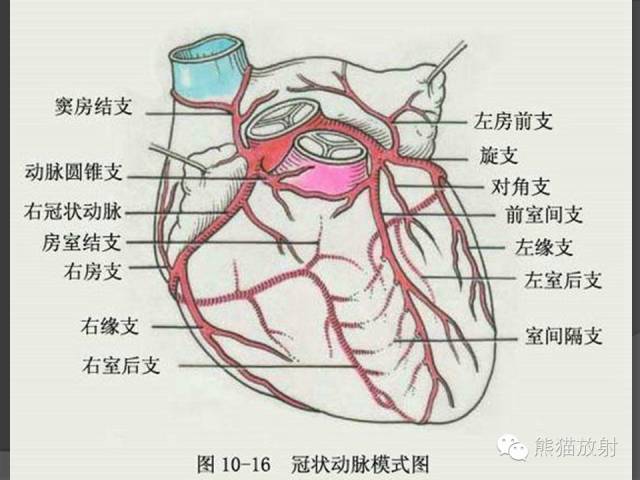
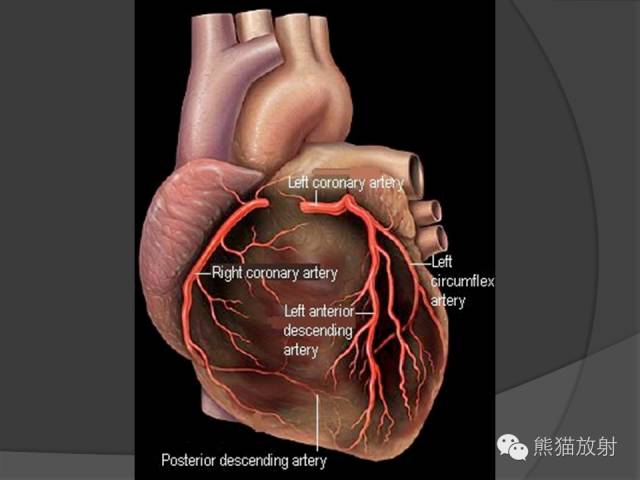
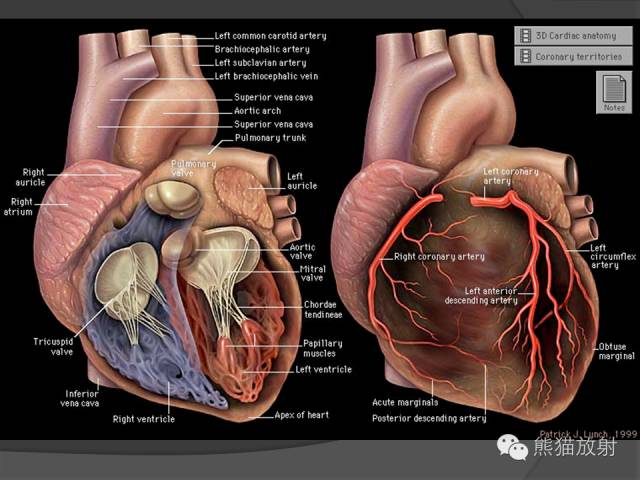
心脏系统解剖图
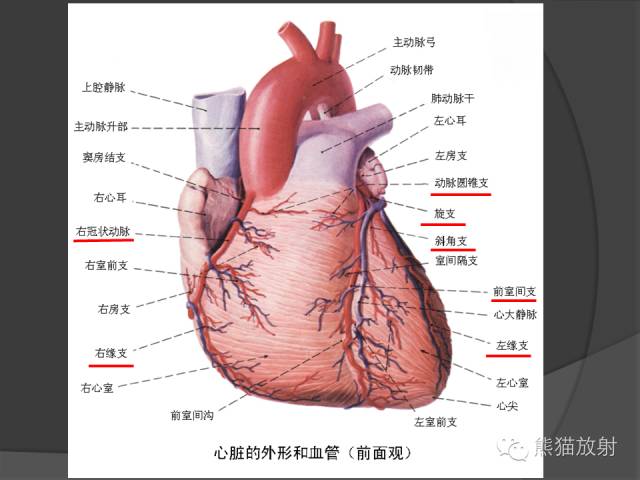
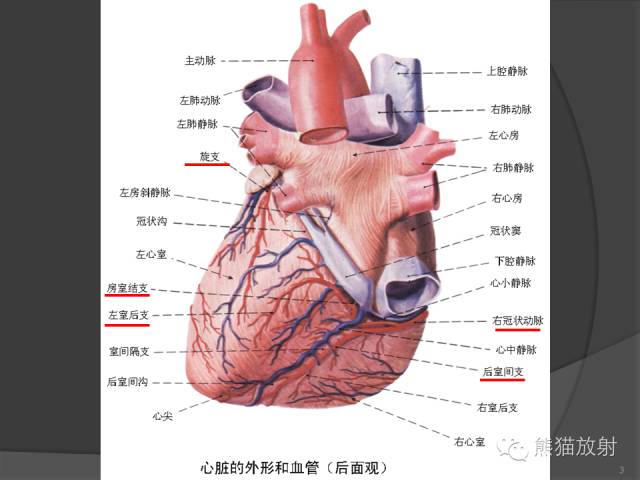
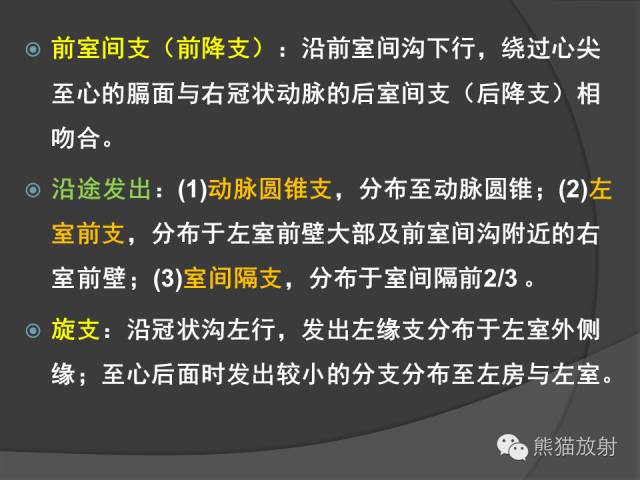
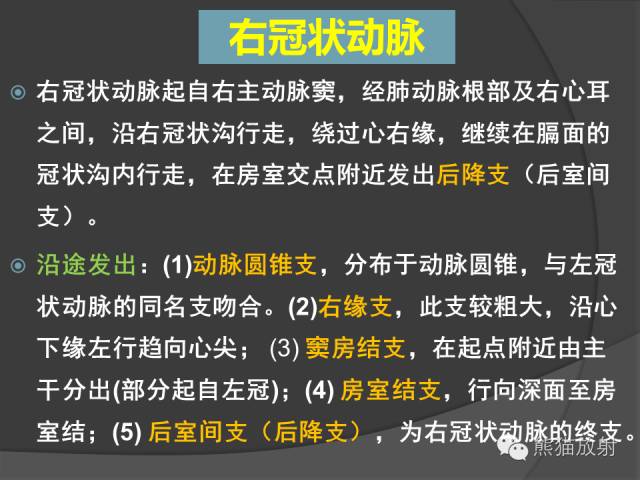
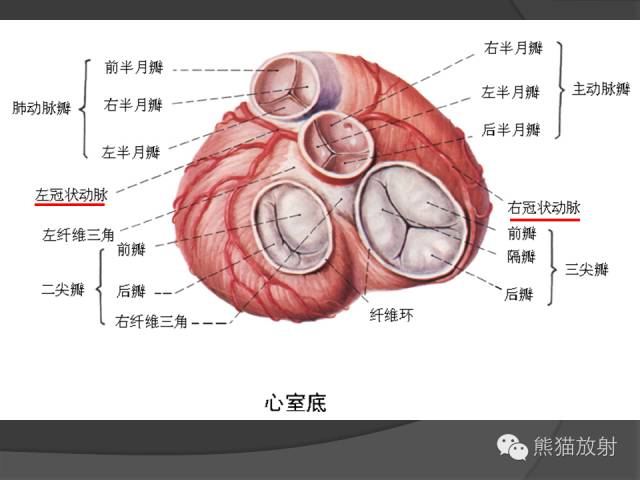 左、右冠状动脉介绍
左、右冠状动脉介绍

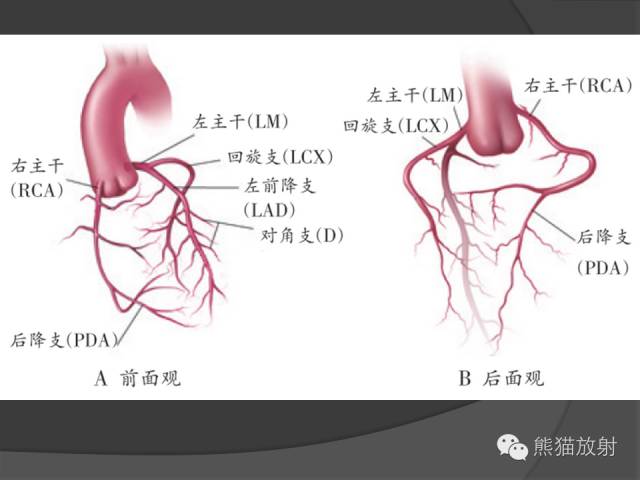
冠状动脉分支解剖
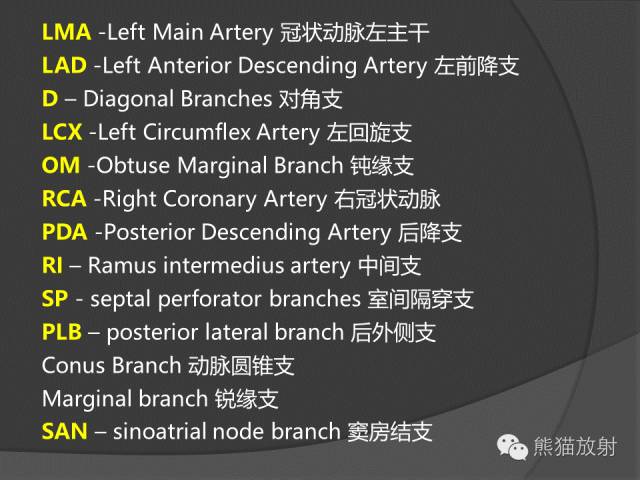
 心血管名称缩写
心血管名称缩写


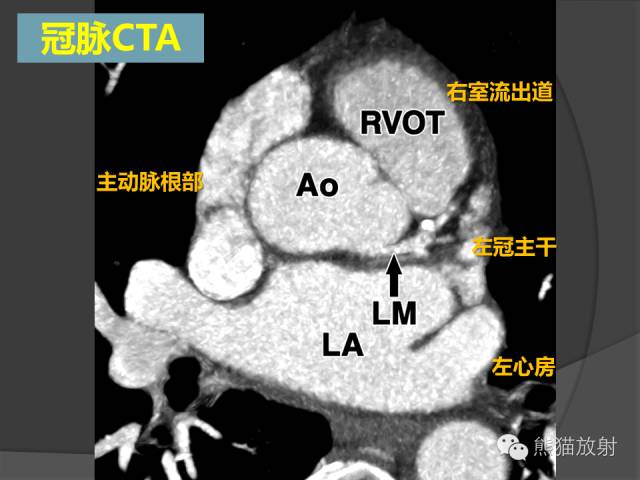
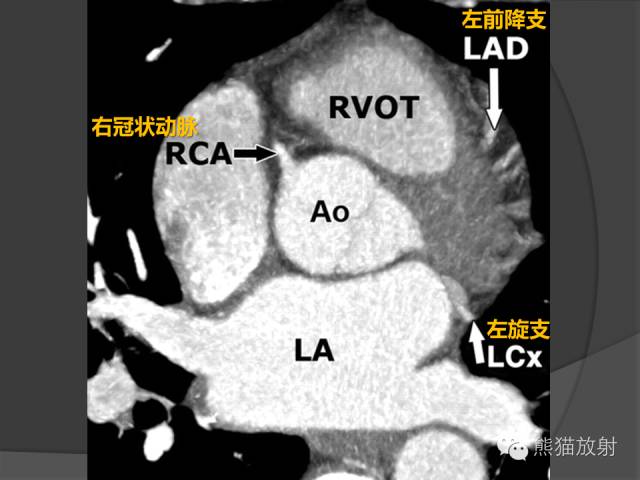
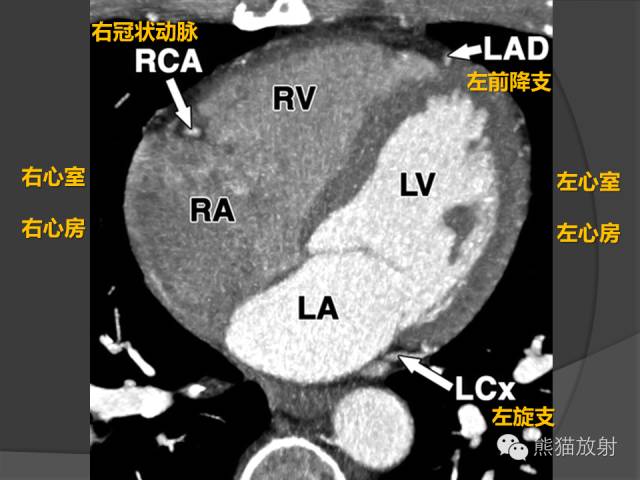
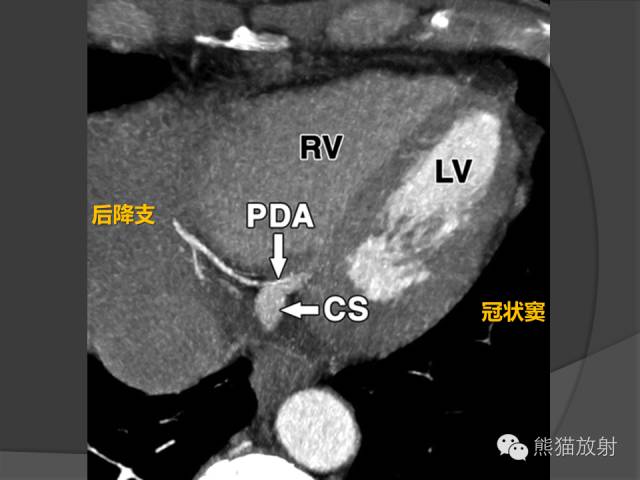
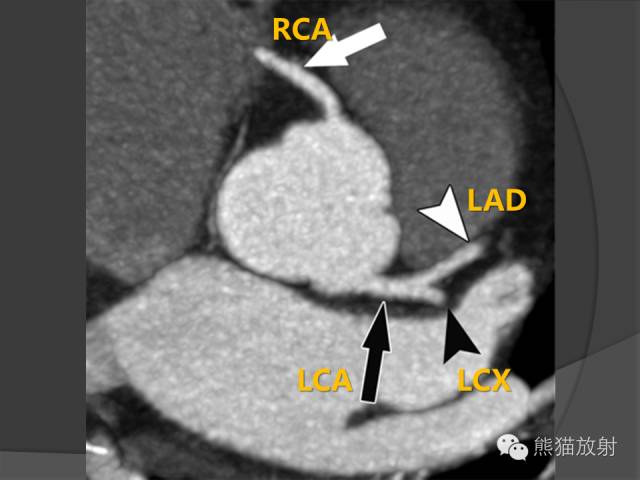
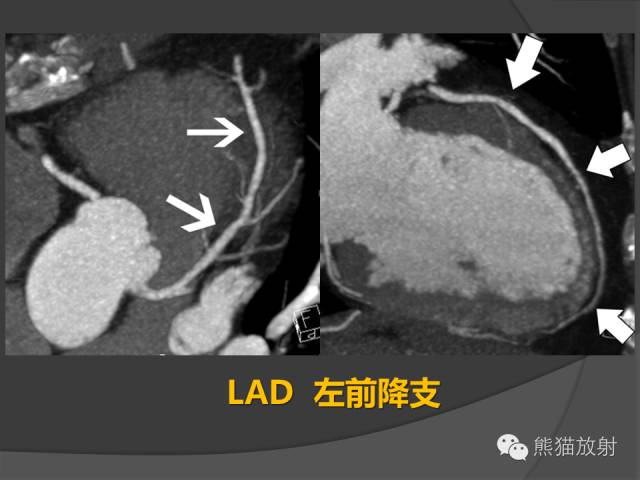
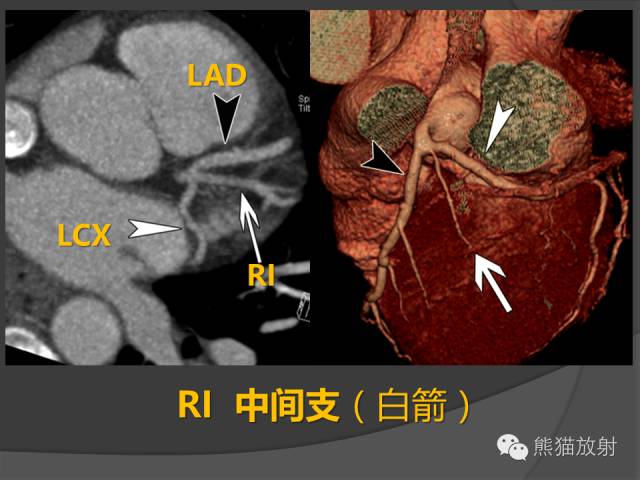
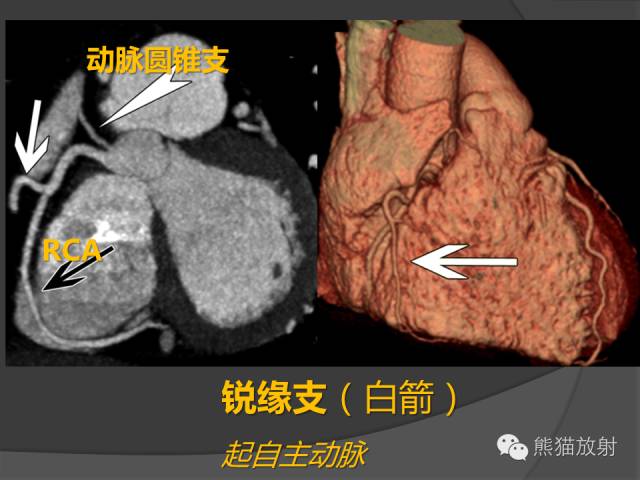
 冠状动脉CTA解剖
冠状动脉CTA解剖


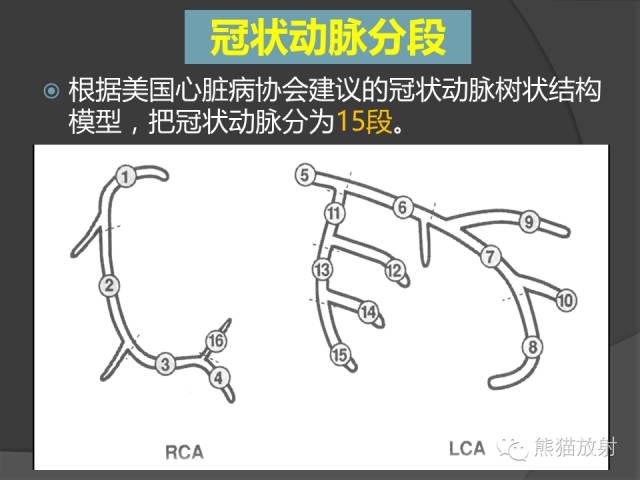
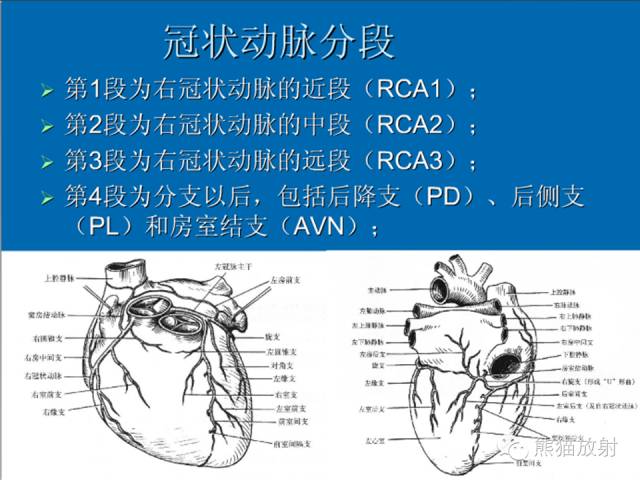
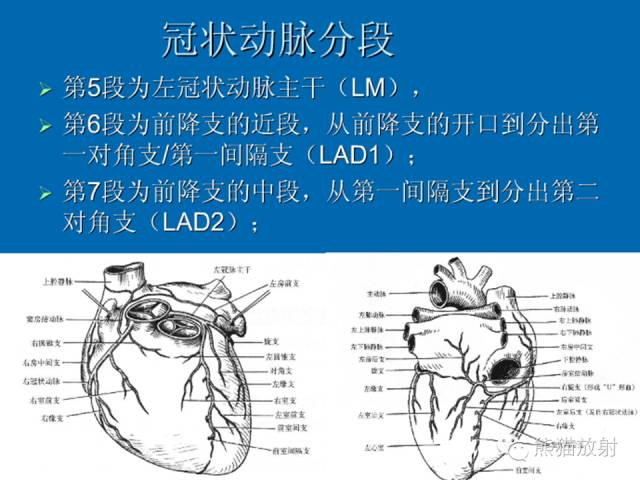
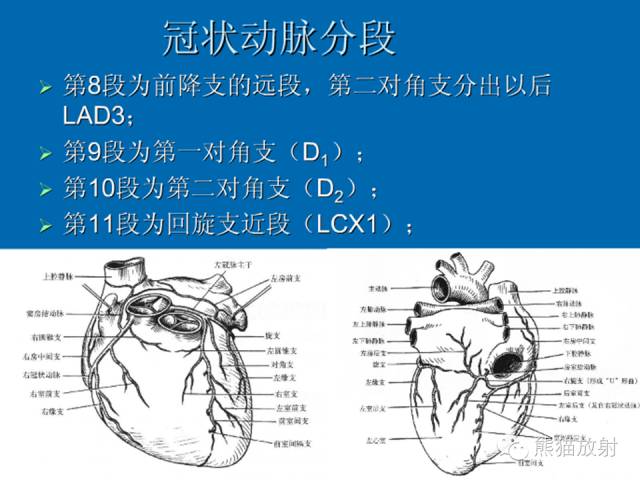
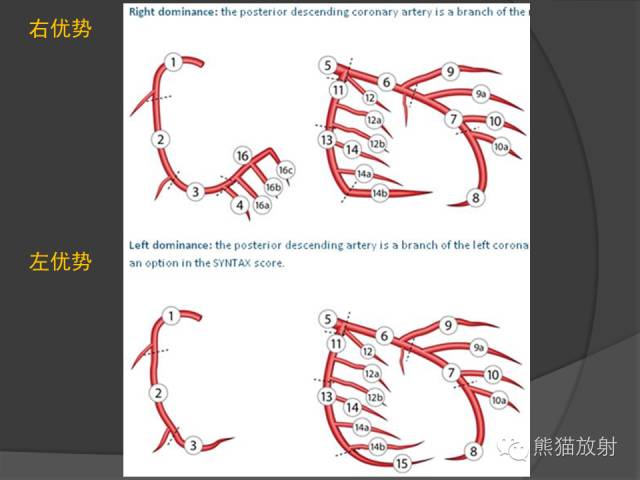
 冠状动脉分段方法
冠状动脉分段方法

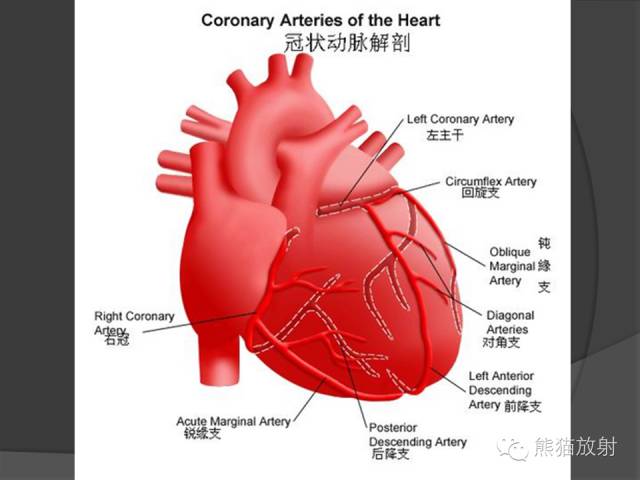
英文解剖图
上述资料整理自网络及个人收藏,不当之处请指教。
LMA 冠状动脉左主干
LAD 左前降支
D 对角支
LCX 左回旋支
OM 钝缘支
RCA 右冠状动脉
PDA 后降支
RI 中间支
PLB 后外侧支
引申阅读:BMJ:冠脉CT vs 冠脉造影,孰优孰劣?
来自德国的研究人员开展了一项前瞻性随机化单中心研究,该研究的目的是评估有中等概率冠状动脉疾病的患者是否应该接受有创冠状动脉造影或计算机断层扫描(CT)。该研究在德国的大学医院进行。
该研究共包括340例疑似冠状动脉疾病患者,基于非典型心绞痛或胸痛具有冠状动脉造影的临床适应症。
患者被随机分配,168例接受CT,172例接受冠状动脉造影。随机化后,1例患者拒绝CT,10例患者拒绝接受冠状动脉造影,最后剩余167例患者(88名女性)和162例患者(78名女性)可进行分析。
主要结果是CT或血管造影最后相关程序后48小时内的主要手术并发症。
心脏CT将冠状动脉造影的需要从100%降至14%(95%置信区间9%至20%,P <0.001),并且冠状动脉造影有显著更高的诊断率:75%(53%至90% )vs 15%(10%至22%),P<0.001。主要手术并发症并不常见(0.3%),组间发生率都是相似的。CT组的轻度手术并发症发生率要低于冠状动脉造影组:3.6%(1%至8%)vs 10.5%(6%至16%),P=0.014。CT将血管造影术组的平均时间长度从52.9小时(四分位数范围49.5-76.4小时)缩短至30.0小时(3.5-77.3小时,P<0.001)。在CT和血管造影术组之间,暴露的总辐射是相似的:5.0mSv(四分位数范围4.2-8.7mSv)vs 6.4mSv(3.4-10.7mSv),P=0.45。在中位随访3.3年后,CT组167例患者中的7例患者(4.2%)和冠状动脉造影组162例患者中的6例患者(3.7%)发生了严重不良心血管事件(调整后的危险比为0.90,95%置信区间0.30至2.69,P=0.86)。79%的患者表示他们更喜欢接受CT测定。该研究是在德国的大学医院进行,因此在常规临床实践中CT的性能可能不同。患病率低于预期,这就导致预定义的主要结果的研究不充分。
相对于冠状动脉造影来说,CT提高了诊断率,且是一种安全的无创诊断方式,并且没有增加长期事件发生率。CT将持续时间缩短了22.9小时,患者优先选择非侵入性测试。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







不错,学习了。
46
认真学习了
49
棒
58
优秀啊 学习了
42
冠状动脉系统
45