SCI REP:肺癌DC细胞的STAT3以及NF-κB通路抑制
2017-03-29 MedSci MedSci原创
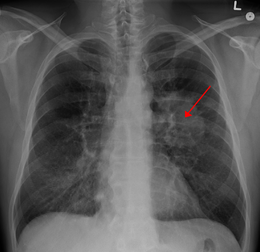
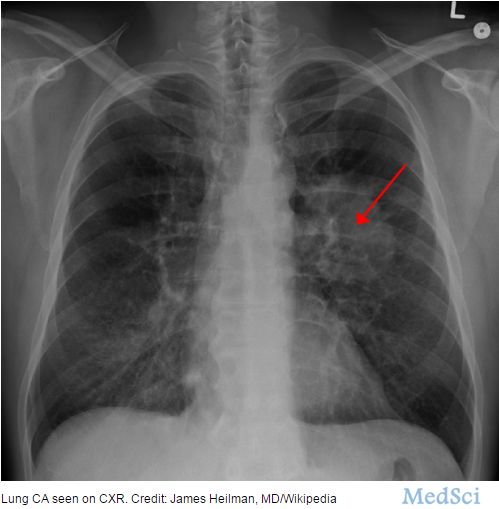
肺癌是世界范围内最常见的恶性肿瘤之一,超过80%为非小细胞肺癌。DC细胞对于继发免疫反应至关重要,在肿瘤发展过程中DC细胞的抗原识别呈递功能受限,肿瘤诱导DC细胞耐受被认为是肿瘤进展侵袭的关键因素,但是肿瘤细胞诱导DC细胞功能缺损的机制尚不清楚。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#STAT3#
0
#DC细胞#
43
学习了
68
谢谢分享,学习了。
60