Circ Arrhythm Electrophysiol:隐性脑卒中患者心电监护时间越长,房颤检出率越高?
2015-02-05 MedSci MedSci原创
卒中会导致残疾的发生,也是全球死亡第二位的最常见病因。房颤导致的心源性栓塞是缺血性脑卒中发生的主要原因。虽然房颤的预防和治疗已经收到了显著的关注,对突发性房颤是否会导致隐源性缺血性卒中和短暂缺血性卒中的研究是一项重大的挑战。卒中和短暂缺血性卒中后房颤的诊断率为10%,当进行30天的心电监护后,诊断率增加了11%。但是,对于未有明显症状的患者和发作时间较长的患者而言,通过心电监护检测突发性房颤非
卒中会导致残疾的发生,也是全球死亡第二位的最常见病因。房颤导致的心源性栓塞是缺血性脑卒中发生的主要原因。虽然房颤的预防和治疗已经收到了显著的关注,对突发性房颤是否会导致隐源性缺血性卒中和短暂缺血性卒中的研究是一项重大的挑战。卒中和短暂缺血性卒中后房颤的诊断率为10%,当进行30天的心电监护后,诊断率增加了11%。但是,对于未有明显症状的患者和发作时间较长的患者而言,通过心电监护检测突发性房颤非常困难。因此,加拿大魁北克谢布克大学Dussault C等人,研究了隐性脑卒中或短暂学缺血性脑卒中后心电监护时间长短与房颤检出率之间的联系,研究成果发表在1月份Circulation Arrhythmia and electrophysiology期刊上。
背景:房颤是卒中发生的主要病因。心电监护检测房颤的最佳时间目前还不是非常清楚。研究进行了系统回顾和Meta分析,从而探讨缺血事件发生后,进行心电监护的时间长短是否跟房颤的检出率有关。
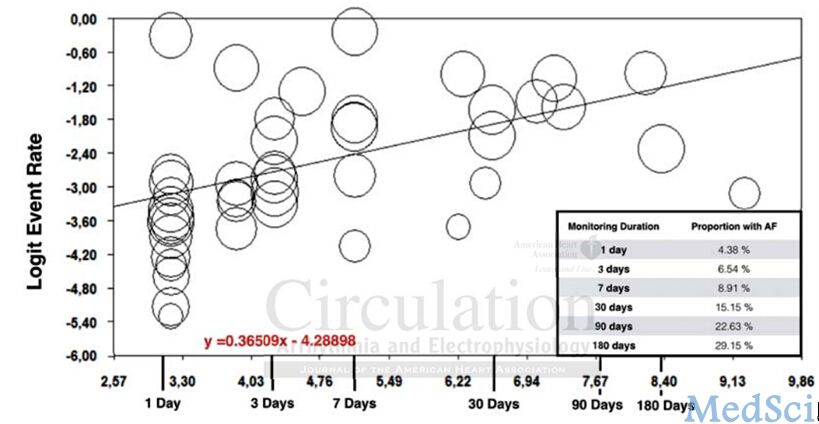
方法和结果:纳入标准:纳入新诊断缺血性卒中或短暂性缺血性脑卒中后至少进行长于12小时心电监护患者,剔除出血性的中风或者以前就已经诊断房颤的患者,共31篇文章符合纳入标准。将心电监护时间作为连续变量,发现监护时间越长,其对于房颤的疹出率越高(P<0.001Meta回归分析)。基于心电监测时间的二分法研究,发现监护时间少于72小时的房颤检出率为5.1%,而监护时间长于7天的房颤检出率为15%。而超过3个月的心电监护,其房颤检出率提高到了29.15%。两组之间有着显著的异质性(≤72 小时: I2 = 91.3%; ≥7 天: I2 = 75.8%)。评估了3项随机对照研究的房颤检出率,发现进行长期监测的患者,其检出率提高7.26%(95% 可信区间[3.99-12.83]; p <0.001)。
结论:隐性脑卒中患者,其心电监护时间越长,房颤的检出率越高。若要决定心电监护的最优时间,仍然需要进一步的研究。
原文出处:
Dussault C, Toeg H, Nathan M, Wang ZJ, Roux JF, Secemsky E. Electrocardiographic Monitoring for Detecting Atrial Fibrillation after Ischemic Stroke or Transient Ischemic Attack: A Systematic Review and Meta-Analysis. Circulation Arrhythmia and electrophysiology. 2015.
本文是MedSci编译,欢迎转载,转载请注明出处,非常感谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#脑卒中患者#
28
#卒中患者#
24
#检出率#
31
#Physio#
23
已阅
113
已阅
115
#监护#
26
Mark
130