NICE指南:儿童胃食管反流病
2015-01-28 doctorpacino 丁香园
胃食管反流是一种正常的生理现象,但是当其可致严重症状而需治疗或引起并发症时则称为胃食管反流病(GORD)。在婴幼儿和儿童中,由于存在各种潜在症状且缺乏简单可靠、能广泛使用的诊断性检测方法,故难以鉴别生理性胃食管反流和病理性胃食管反流病,这会导致极大的临床实践差异。 该病可影响儿童,包括早产和足月新生儿、健康婴幼儿和儿童及确定有明确危险因素的患儿,如膈疝修补术后、其他先天性畸形、严重的
胃食管反流是一种正常的生理现象,但是当其可致严重症状而需治疗或引起并发症时则称为胃食管反流病(GORD)。在婴幼儿和儿童中,由于存在各种潜在症状且缺乏简单可靠、能广泛使用的诊断性检测方法,故难以鉴别生理性胃食管反流和病理性胃食管反流病,这会导致极大的临床实践差异。
该病可影响儿童,包括早产和足月新生儿、健康婴幼儿和儿童及确定有明确危险因素的患儿,如膈疝修补术后、其他先天性畸形、严重的神经系统功能障碍;有明确危险因素可能存在复杂合并症的儿童。近期BMJ杂志发布了NICE(英国国家卫生与临床优化研究机构)最新指南,详细阐述了婴幼儿、儿童和青少年胃食管反流病的识别、诊断和管理。
一、胃食管反流病的诊断与检查
1.进食后引起的反流是一种常见且正常的现象:由胃食管反流引起,是婴幼儿期一种正常的生理过程;通常不需要任何检查或治疗;通过给予父母和看护人员一些建议与鼓励即可控制症状。(基于来自观察性研究的高、中、低级别证据以及指南制定工作组的经验和意见)
2.需要注意的是,在少部分婴幼儿中,胃食管反流可能与易激惹有关,或可导致某些明显并发症并需要临床干预,这被称为胃食管反流病。
3.胃食管反流的建议以及健康婴幼儿出现进食后反流时给与父母和看护人员安慰:该症状很常见(至少发生于40%的婴幼儿);通常在婴幼儿出生后8周内出现;可能会频繁出现症状(受该症状影响的儿童中约有5%患儿发生的频率≥6次/天);症状通常随着时间而缓解(受该症状影响的孩子中有90%会在1岁前缓解);通常不需要进一步的检查或者治疗。
4.安慰父母和看护人员时,建议他们:如果出现以下任何情况,需要带着孩子复诊:反流变成持续性喷射状呕吐;呕吐物含有胆汁(绿色或者黄绿色)或者呕血(呕吐物中带血);有新症状出现,如明显的易激惹症状、喂养困难或生长发育迟缓;出生一年后仍然出现持续频繁的反流症状。
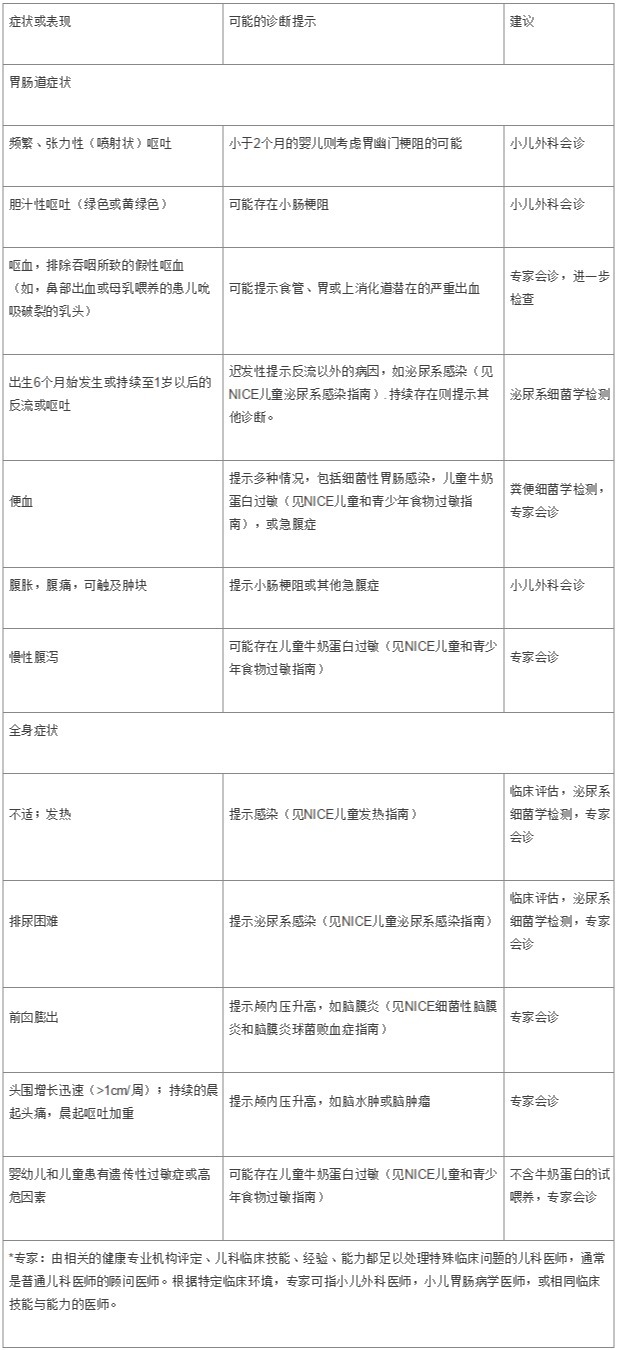
5.在呕吐或者反流的婴幼儿、儿童和青少年中,注意观察”红旗”症候群(red flag)症状,这可能提示除胃食管反流外的一些功能紊乱疾病。通过临床判断进一步检查或者会诊。
6.如果婴幼儿或者儿童没有出现明显的反流症状而仅呈现以下其中之一时,无需定期检查或者治疗:无法解释的喂养困难(如拒食,恶心,或窒息);易激惹;生长发育迟缓;慢性咳嗽;声嘶;肺炎发生。
7.在婴幼儿、儿童和青少年中, 辨别胃食管反流可能存在的并发症:反流性食管炎;反复发作的吸入性肺炎;频繁发作的中耳炎(如6个月内发生3次以上);在神经功能障碍特别是脑瘫患儿中出现牙蚀症。
8.在儿童和青少年中,辨别胃食管反流可能表现的症状:烧心;胸骨后疼痛;上腹部疼痛。
9.需注意胃食管反流在哮喘儿童和青少年中更常见,但是尚无证据证明胃食管反流能引起或加重哮喘。
10.需要注意的是,某些非IgE介导的牛奶蛋白过敏反应与GORD症状类似,特别是在有遗传性过敏症状、体征或者家族史(或者联合出现)的婴幼儿中。如果怀疑非-IgE介导的牛奶蛋白过敏反应,请参考NICE儿童和青少年食物过敏指南。
11.当决定是否进行检查或者治疗时,请考虑以下导致GORD患病率增加的因素:早产;亲代病史中存在烧心或者反酸;肥胖;食管裂孔疝;先天性膈疝病史(修补术后);先天性食管闭锁病史(修补术后);神经功能障碍。
12.对于肥胖并且伴有烧心或者反酸症状的儿童和青少年,建议他们和他们的父母以及看护人员减肥,对改善症状或有帮助。
13.出现持续性背部反弓或者表现为Sandifer综合征(颈部过伸与旋转而出现节段性斜颈)的婴幼儿和儿童,需要进行专家评估。
14.胃食管反流罕见引起呼吸暂停多次发作或者明显的危及生命的事件发生,但是如果在普通儿科评估后认为胃食管反流是引起以上两种情况的可疑因素,需要考虑转诊至专家门诊进一步检查。
15.婴幼儿或儿童无需行上消化道造影来诊断GORD或者评估GORD的严重程度。上消化道造影可用于原因不明的胆汁性呕吐(尤其是婴幼儿)或者吞咽困难。
16.对于年龄<2个月的婴儿,若出现呕吐进行性加重或张力性呕吐时,需要当日安排专科医院行急诊评估,以确定可能存在的肥厚性幽门狭窄。
17.胃食管反流的婴幼儿若有以下表现,需要检查尿路感染的可能性:生长发育迟缓;迟发性反流(出生8周以后)反流频繁发作和易激惹。
二、胃食管反流与GORD的初步处理
1.睡眠中的婴幼儿不宜使用体位疗法,与NHS建议一致。婴幼儿睡眠时应采用仰卧位。
2.母乳喂养的婴幼儿若出现频繁反流症状且易激惹时:确保有人获取专门的知识和训练以评估母乳喂养情况;母乳喂养评估和建议之后仍然出现持续的易激惹,可考虑试验性使用藻酸盐1-2周。若药物治疗有效,停止使用,并观察停药后的恢复情况。
3.配方奶喂养的婴幼儿若出现频繁反流症状且易激惹时,可使用以下阶梯疗法。回顾喂养史:如果婴幼儿体重超重,则减少喂养总奶量;少量多餐喂养(保证合适的每日需要总量),直至喂养的足够少量而频繁;喂养稠厚食物(如:富含大米淀粉、玉米淀粉、豆角胶、卡罗布胶);若阶梯疗法无效,停止稠厚食物喂养,试验性使用藻酸盐1-2周。若药物治疗有效,停止使用,并观察停药后的恢复情况。
三、胃食管反流病的药物疗法
1.婴幼儿和儿童的明显胃食管反流作为孤立症状存在时,不使用抑酸剂,如质子泵抑制剂(PPIs)或组胺H2受体拮抗剂。
2.无法清楚描述症状的患儿(如婴幼儿和年龄较小的儿童,神经功能障碍所致交流沟通困难的患儿),出现明显的胃食管反流症状且合并以下一项或多项情况时,可考虑给予4周的质子泵抑制剂(PPIs)或组胺H2受体拮抗剂治疗:无法解释的喂养困难(如拒食,恶心,或窒息);易激惹;生长发育迟缓。
3.儿童和青少年出现持续烧心、胸骨后疼痛或上腹痛时,可考虑使用4周的质子泵抑制剂治疗。
4.使用质子泵抑制剂(PPIs)或组胺H2受体拮抗剂治疗达4周时评估疗效,若出现以下情况可考虑进一步专家评估或者内镜检查:症状无缓解;停药后复发。
5.选择质子泵抑制剂(PPIs)还是组胺H2受体拮抗剂,需考虑:药物适用年龄;父母(或看护人员)、儿童、青少年的偏好;当地治疗所花费用。
6.经内镜确诊的婴幼儿、儿童或青少年反流性食管炎可使用质子泵抑制剂(PPIs)或组胺H2受体拮抗剂治疗,考虑重复行内镜检查是必须的,以指导下一步治疗方案。
7.没有专家医师的指导意见,不使用甲氧氯普胺、多潘立酮、红霉素治疗胃食管反流或GORD。需考虑这些药物可能发生的副作用。
四、胃食管反流病的手术治疗
1.婴幼儿、儿童或青少年严重难治性GORD出现以下情况时可考虑胃底折叠术治疗:药物治疗无效,或成分喂养治疗GORD不现实——如,长期、持续、稠厚的肠内营养方式。
2.关于肠内营养和手术治疗的更多推荐可以才参考下面的信息附录2。
五、更多推荐
1.上消化道对比造影:
不建议婴幼儿、儿童或者青少年行上消化道造影来诊断GORD或者评估GORD的严重程度;婴幼儿出现胆汁性呕吐时行急诊(同一天)上消化道对比造影检查。向父母或看护人员解释患儿需排除肠旋转不良所致的小肠梗阻等严重疾病;儿童或者青少年有吞咽困难病史者可行上消化道对比造影检查。
2.内镜和食管pH值测定/食管测压:
建议相关婴幼儿、儿童或者青少年至专科机构行上消化道内镜检查与活检:呕血(呕吐物为血性)、排除吞咽血性物质引起的假性呕血(出现临床症状的同一天即行该检查;见表1)、黑便(黑色,恶臭粪便)(出现临床症状的同一天即行该检查;见表1)、出生1年后症状无改善、明显的反流症状导致生长发育迟缓、有沟通障碍的儿童和青少年出现无法解释的易激惹、胸骨后、剑突下或上腹部疼痛,需要进一步治疗或者对治疗不敏感、厌食且有反流病史、无法解释的缺铁性贫血、有胃底折叠术适应症。
考虑行食管pH值测定(或食管pH值测定联合食管测压技术):吸入性肺炎可疑复发;无法解释的窒息;无法解释的非癫痫样发作;与神经功能障碍相关的牙蚀症;反复发作的中耳炎;可能需要行胃底折叠术的情况(参考“术前检查”第二点);怀疑Sandifer’s 综合征。
考虑行食管pH值测定而不行食管测压,能保证有效的抑酸治疗。
3.GORD的肠内营养:
明显胃食管反流的婴幼儿和儿童出现生长缓慢时可考虑肠内营养以促进体重增长:存在体重增长缓慢的其他病因,或针对胃食管反流的喂养建议和医学干预无效。
明显胃食管反流的婴幼儿和儿童出现生长缓慢时行肠内营养之前需考虑的:个体化营养支持计划;尽快减少肠内营养的措施;合适的情况下尽快撤除肠内营养的措施。
明显胃食管反流的婴幼儿和儿童出现生长缓慢时接受肠内营养:提供经口喂养,能够耐受时不能中断经口喂养;遵循营养支持计划,保证能达到预期目标体重并保持合适体重;尽快减少和停止肠内营养。
婴幼儿、儿童和青少年的空肠营养:需要肠内营养且无法耐受经胃营养的情况,如反流,或者担心反流导致的吸入性肺炎。
4.术前检查:
怀疑婴幼儿、儿童和青少年患有GORD,决定何时行胃底折叠术时,可行上消化道内镜检查和活检。决定何时行胃底折叠术时,还可考虑其他一些检查,如食管pH值测定(或食管pH值测定联合食管测压技术),上消化道对比造影检查。
表1 婴幼儿和儿童“红旗”症候群,提示除胃食管反流以外的疾病

信息附录1:指南中使用的定义
胃食管反流:胃内容物反流入食管,是一种常见的生理现象,可以发生于从婴儿到老年人的任何年龄,经常无明显症状,喂养或进食后加重。大部分婴幼儿表现为“显而易见的反流”——喂养后看得见的反流物。
胃食管反流病:胃食管反流引起严重症状(如不适和疼痛)或并发症(如食管炎和吸入性肺炎)且需要医疗干预时称为胃食管反流病。成人使用此名称通常指更狭窄的含义,特指反流性食管炎。
易激惹:证据有限,没有客观或者广泛接受的临床定义,包含婴幼儿和儿童不能充分表达他们感觉到的情绪。在本指南中,易激惹指外在疼痛或不愉快的外向性表达,是经过合适的训练能够胜任专业医疗保健的人员在全面评估的基础上仍无法评估的一种状态。易激惹的评估需详细分析父母和看护人员提供的每个个体儿童的情况描述。
信息附录2:指南的进一步说明
1.胃食管反流病指南路径真实呈现了NICE所有的推荐,在NICE官网可以找到(http://pathways.nice.org.uk/pathways/dyspepsia-and-gastro-oesophageal-reflux-disease)。
2.NICE路径为社会健康和福利专家、公众健康专家、社会健康和福利机构提供者或行政长官、社会民众提供帮助。完成指南实施的审核和成本计算工具可在官网找到(www.nice.org.uk/guidance/NG1/resources)。
3.父母、儿童和青少年也可通过相应的NICE公开信息获得指导 (www.nice.org.uk/guidance/NG1/informationforpublic)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








不错的指南,为我们探讨研究提供了方针,给点个赞了!
0
儿科的,学习一下
68
继续学习
70
继续关注
58
值得深入研究
109
#反流病#
27
#胃食管#
32
#胃食管反流#
36
#NICE#
25
#食管#
21