WCIO:地塞米松和福沙吡坦可以降低DEB TACE术后PES风险
2016-06-16 Seven L 译 MedSci原创
根据介入肿瘤学世界会议的报告,对原发性肝癌(HCC)患者进行药物洗脱珠肝动脉化疗栓塞术 (DEB TACE) 前联合使用Decadron和Emend,可以预防患者治疗后的栓塞后综合征。辛辛那提大学介入放射学助理教授Abouelmagd Makramalla博士和同事对71名进行DEB TAC的HCC患者进行了研究。一共涉及113个操作,所有患者在术前通过静脉注射8 mg of Decadron(地
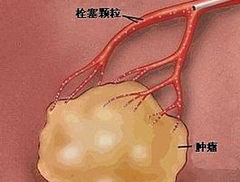
根据介入肿瘤学世界会议的报告,对原发性肝癌(HCC)患者进行药物洗脱微粒肝动脉化疗栓塞术 (DEB TACE) 前联合使用Decadron和Emend,可以预防患者治疗后的栓塞后综合征。
辛辛那提大学介入放射学助理教授Abouelmagd Makramalla博士和同事对71名进行DEB TACE的HCC患者进行了研究。一共涉及113个操作,所有患者在术前通过静脉注射8 mg of Decadron(地塞米松,Merck)和150 mg of Emend (福沙吡坦, Merck)。研究目标是确定这种用药方案能都降低栓塞后综合征(PES)的风险。PES可以在术后72小时内引起发烧、恶心、呕吐、疼痛等不适。
数据显示,有4.4%(n = 5)的患者入院时有PES,随后DEB TACE治疗;99名患者不需要住院或急诊就诊;9名患者因为非PES原因入院。
研究人员总结说,“门诊进行DEB TACE前使用地塞米松和福沙吡坦治疗是可行的,能降低患者因PES的入院率。”
原始出处:
Young C, et al. Abstract #. Presented at: World Conference on Interventional Oncology; June 9-12, 2016; Boston.
Decadron plus Emend reduces PES after drug eluting bead TACE for HCC.Healio.June 15, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ACE#
34
#PE#
25
#TAC#
37
#福沙吡坦#
34