Radiology:COVID-19感染患者康复一年后存在持续性脑白质微结构改变
2021-12-23 影像小生 MedSci原创
新冠肺炎临床康复患者1年后轴突密度较低。住进重症监护室的病人有更多的白质异常。康复患者认知功能无明显下降。住院时间可能是一年后随访白质变化的预测因子。
越来越多的证据表明,严重急性呼吸综合征冠状病毒可影响中枢神经系统。然而,关于在一年的随访中白质和认知后遗症的数据是缺乏的。
中南大学湘雅二医院放射科刘军教授团队、呼吸与危重症医学科罗红教授团队进行了相关研究,并在BRAIN杂志发表研究论文。
该研究调查了22名COVID-19康复者和21名匹配的健康对照组。采用弥散张量成像(DTI)、弥散峰度成像(DKI)、神经突起方向离散度与密度成像(NODDI)识别白质变化,采用韦氏智力量表亚量表评估认知功能。然后检查弥散指标、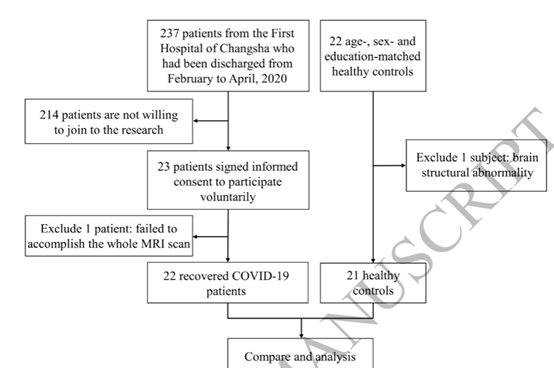
认知功能和其他临床特征之间的相关性。另外还基于患者是否入住ICU,还进行了亚组分析,
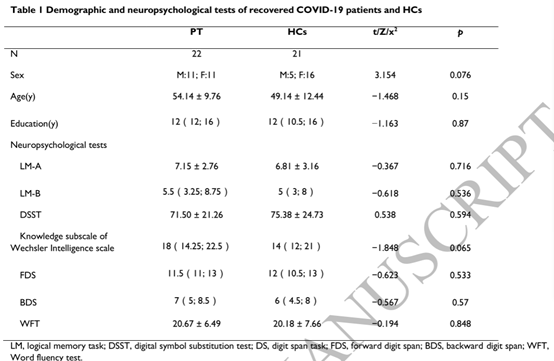
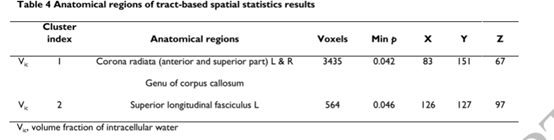
康复组放射冠、胼胝体和上纵束细胞内水体积分数低于健康对照组。ICU患者胼胝体的各向异性分数比非ICU患者低。与健康对照组相比,康复组患者认知功能无明显下降。

随着住院时间的缩短和随访时间的延长,白质倾向于出现更少的异常。
该研究使用常规DTI指标以及DKI和NODDI模型,全面调查了康复COVID-19患者在一年随访中的WM变化。康复后一年的COVID-19的Vic值低于HCs。此外,ICU患者白质异常稍多。与健康对照组相比,康复的COVID-19患者的认知功能没有明显下降。最后,在较短的住院时间和较长的随访时间内,白质倾向于呈现较少的异常。
原文出处
Huang S, Zhou Z, Yang D, et al. Persistent white matter changes in recovered COVID-19 patients at the 1-year follow-up [published online ahead of print, 2021 Dec 16]. Brain. 2021;awab435. doi:10.1093/brain/awab435
https://academic.oup.com/brain/advance-article/doi/10.1093/brain/awab435/6464331
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#微结构#
59
#持续性#
72
#白质#
42
#新冠肺炎# 很重要的发现
171
实用
65