Heart:氧化应激增强和心室动脉瘤可预测心脏结节病风险
2022-01-27 MedSci原创 MedSci原创
U-8-OHdG水平和伴有VA是心脏结节病患者首次发生持续性室性心动过速/心源性猝死的强有力的预测因子,这有助于心脏事件的分层并提供有关室性心动过速的相关信息。
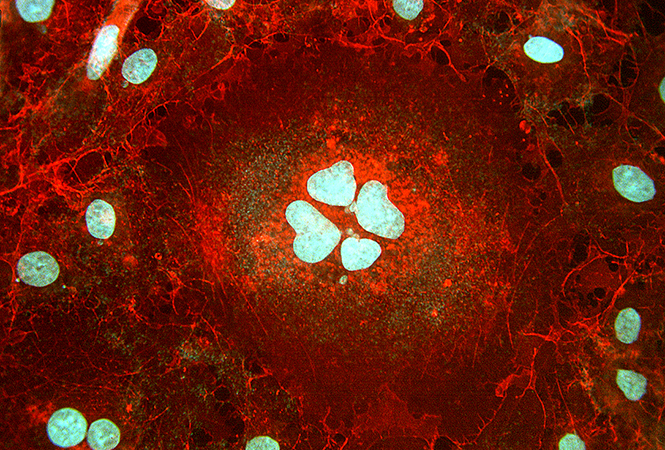
结节病是一种全身性炎症性疾病,其特征是病因不明的非干酪样上皮样肉芽肿。心脏结节病患者预后不良,常伴有心力衰竭(HF)、高度房室传导阻滞和室性心律失常,其中心源性猝死是导致心脏结节病死亡的主要原因。
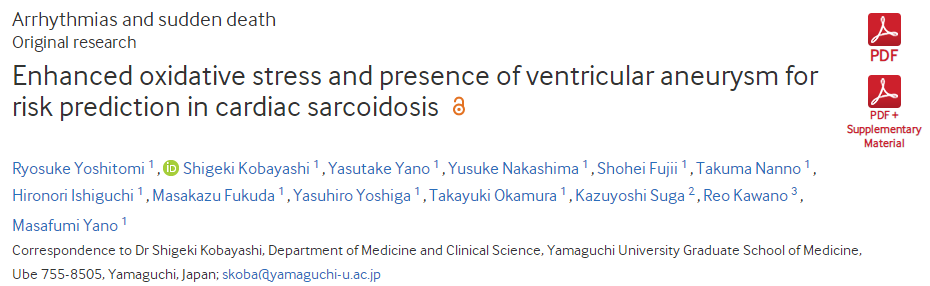
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员旨在明确心脏结节病患者持续性室性心动过速和心源性猝死的预后标志物。
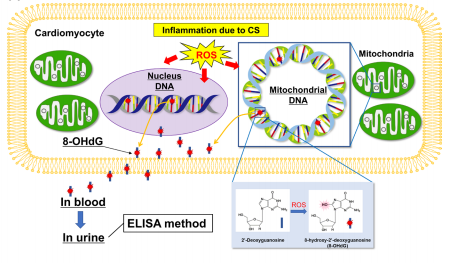
研究人员对2008年6月至2020年3月期间在研究人员所在医院根据日本或心律学会指南诊断为心脏结节病患者进行了一项前瞻性观察性队列研究。该研究的主要终点是第一次持续性室性心动过速和心源性猝死的复合结局。在参与者入院时测量了尿中8-羟基-2'-脱氧鸟苷(U-8-OHdG)水平,这是一种反映心脏结节病炎症活性的氧化性DNA损伤的标志物,同时检测了其他生物标志物和心肾功能指标。
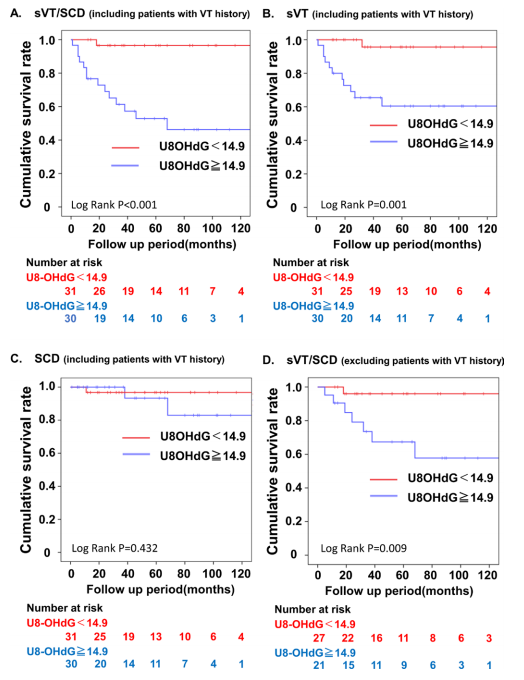
该研究纳入了连续就诊的89例心脏结节病患者。研究人员排除了28名在心脏中没有异常18F-氟脱氧葡萄糖(18F-FDG)积累的患者。研究人员对61名18F-FDG积累异常的患者进行了中位时间为46个月的随访(IQR为20-84)。在随访期间,61名患者中有15名患者出现了持续性室性心动过速(n=12)或心源性猝死(n=3)。Cox比例风险模型显示U-8-OHdG浓度和伴有心室动脉瘤(VA)是首次持续性室性心动过速/心源性猝死的独立预测因素。预测首次持续性室性心动过速/心源性猝死的U-8-OHdG临界浓度为14.9ng/mg·Cr。U-8-OHdG浓度≥14.9ng/mg·Cr和VA的患者发生持续性室性心动过速/心源性猝死的风险显著增加。
由此可见,U-8-OHdG水平和伴有VA是心脏结节病患者首次发生持续性室性心动过速/心源性猝死的强有力的预测因子,这有助于心脏事件的分层并提供有关室性心动过速的相关信息。
原始出处:
Ryosuke Yoshitomi.et al.Enhanced oxidative stress and presence of ventricular aneurysm for risk prediction in cardiac sarcoidosis.heart.2022.https://heart.bmj.com/content/early/2022/01/24/heartjnl-2021-320244
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#心脏结节病#
44
#激增#
49
#ART#
38
#应激#
40
#HEART#
43
#学习#预防为主,防治结合
50
真好
0