Cancer Cell:R-ras有助肿瘤血管成熟
2012-08-15 Bryond 生物谷
由于抗癌药物主要通过血液循环达到肿瘤部位,血管发育异常会阻碍药物的递送。近日,桑福德-伯纳姆医学研究所的研究人员发现一种分子能促进肿瘤血管成熟。这一发现可用于帮助杀伤肿瘤的治疗药物更有效地达到靶部位。相关研究论文发表在在8月Cancer Cell杂志上。 为了生存,肿瘤需要血液供应,需要血液提供营养和氧气。要获得供应,癌细胞必须刺激新血管生长,这一过程称为肿瘤血管生成。科学家们们一直试图抑制
由于抗癌药物主要通过血液循环达到肿瘤部位,血管发育异常会阻碍药物的递送。近日,桑福德-伯纳姆医学研究所的研究人员发现一种分子能促进肿瘤血管成熟。这一发现可用于帮助杀伤肿瘤的治疗药物更有效地达到靶部位。相关研究论文发表在在8月Cancer Cell杂志上。

为了生存,肿瘤需要血液供应,需要血液提供营养和氧气。要获得供应,癌细胞必须刺激新血管生长,这一过程称为肿瘤血管生成。科学家们们一直试图抑制血管生成来切断肿瘤的供应来源。但肿瘤血管生成是渗漏的,导致血管发育不成熟以及畸形血管的生成。由于抗癌药物要达到肿瘤组织需经过血液,因此血管发育异常会阻碍药物的运输。
如果不是制止血管生成,我们帮助肿瘤血管成熟,那么我们也许会更彻底地杀伤肿瘤,治疗可能会更有效。这一观点是有悖常理的概念,如今在Cancer Cell杂志上公布的一篇论文中,桑福德-伯纳姆医学研究所研究人员发现一种分子可以促进肿瘤血管的成熟,以此能改善癌症治疗药物的传递。
我们的发现表明这种分子具有解决血管非正常化造成的各种问题,能解决包括低效的药物输送到肿瘤部位等问题,副教授Masanobu Komatsu博士说::关闭或修复肿瘤血管?早期癌肿瘤血管生成疗法旨在杀死养活肿瘤的血管,以此来饿死肿瘤细胞。工程,虽然药物减缓或阻止血管生成的已经有些成功,但肿瘤细胞是出了名地擅长从生存环境中剥夺营养和氧气。因此,抗血管生成的药物、中药对肿瘤血管生成的抑制不足以完全杀伤肿瘤细胞。
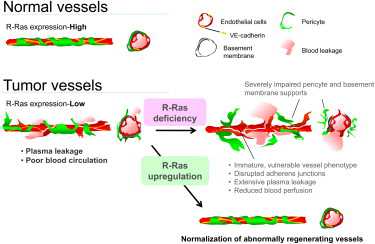
Komatsu等研究人员的战略是基于对一个特定的蛋白质R-ras基因的新认识,团队发现了R-ras基因有助于血管成熟。该蛋白质被发现在正常组织以及成熟的血管中高表达。另一方面,肿瘤的血管通常低表达R-ras基因水平,这是肿瘤血管不成熟的特性之一。
为了深究R-ras基因在肿瘤血管成熟中的重要性,Komatsu和他的团队试图在小鼠体内高表达这一蛋白质。 Komatsu说:因为缺乏R-ras基因,肿瘤血管长期不成熟,我们发现如果我们引进R-ras基因,我们能够改善肿瘤血管的结构和功能,使得血管正常化。Komatsu利用另一种方式即使用R-ras基因,帮助肿瘤血管成熟可能更好地使肿瘤接触到治疗药物。R-ras基因活性的增加也可能有其他好处。如在组织工程、移植组织时,需要充足的血液供应,R-ras基因的高表达能促进功能性成熟血管的生成。
编译自:Protein that helps tumor blood vessels mature could make cancer drugs more effective

doi:10.1016/j.ccr.2012.06.013
PMC:
PMID:
Small GTPase R-Ras Regulates Integrity and Functionality of Tumor Blood Vessels
Junko Sawada, Takeo Urakami, Fangfei Li, Akane Urakami, Weiquan Zhu, Minoru Fukuda, Dean Y. Li, Erkki Ruoslahti, Masanobu Komatsu
We show that R-Ras, a small GTPase of the Ras family, is essential for the establishment of mature, functional blood vessels in tumors. The genetic disruption of R-Ras severely impaired the maturation processes of tumor vessels in mice. Conversely, the gain of function of R-Ras improved vessel structure and blood perfusion and blocked plasma leakage by enhanced endothelial barrier function and pericyte association with nascent blood vessels. Thus, R-Ras promotes normalization of the tumor vasculature. These findings identify R-Ras as a critical regulator of vessel integrity and function during tumor vascularization.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Cell#
40
#肿瘤血管#
35
#cancer cell#
38
#CEL#
38