Nat Immunol:Sox2--从转录因子到免疫卫士
2015-03-23 佚名 生物谷
近日著名的免疫学杂志《自然免疫》发表了中科院生物物理所关于转录因子Sox2在固有免疫中的重要作用:Sox2在中性粒细胞中能够充当胞内DNA传感器的作用,当Sox2结合了细菌DNA后,Sox2会通过激酶TAK1和转接蛋白TAB2介导下游信号通路,开始转录翻译一系列的促炎因子。检测到细胞中的外源核酸并且做出响应是细胞内抗菌系统的重要一环,细胞的固有免疫系统通常会装配有模式识别受体(patt
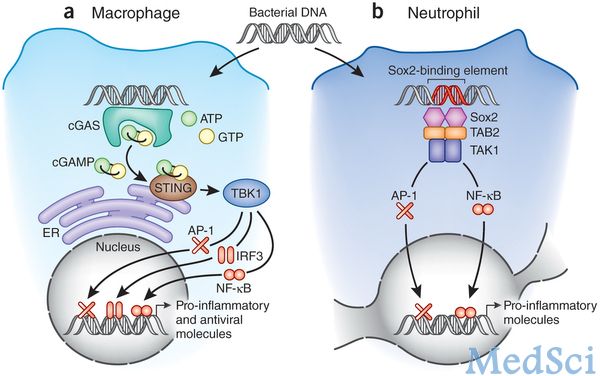
近日著名的免疫学杂志《自然免疫》发表了中科院生物物理所关于转录因子Sox2在固有免疫中的重要作用:Sox2在中性粒细胞中能够充当胞内DNA传感器的作用,当Sox2结合了细菌DNA后,Sox2会通过激酶TAK1和转接蛋白TAB2介导下游信号通路,开始转录翻译一系列的促炎因子。
检测到细胞中的外源核酸并且做出响应是细胞内抗菌系统的重要一环,细胞的固有免疫系统通常会装配有模式识别受体(pattern-recognition receptors),这些受体早已经进化并且能够识别那些外源核酸。然而中科院的新发现告诉我们在中性粒细胞中的Sox2亦可以充当模式识别受体的角色,Sox2识别了入侵细菌的双螺旋DNA后,启动激活免疫系统同仇敌忾。
Sox2广泛为人所知是源于2006年日本科学家山中弥生关于诱导干细胞iPS的工作。当时山中弥生小组将包括Sox2在内的c-Myc,Oct-4和KLF4等四个转录因子转到了成体细胞中,成功地诱导出了具有胚胎干细胞特征的细胞,取名为iPS。Sox2和Oct-4一起调控了下游的基因,在这个复杂的转录复合物中,Sox2自身通过HMG域结合了双螺旋DNA小沟中共有的七个碱基对序列。Sox2因而被认为在胚胎发育,干细胞维持和谱系分化中发挥关键作用。
原始出处:
Mankan AK1, Hornung V1.Sox2 as a servant of two masters.Nat Immunol. 2015 Mar 19;16(4):335-6. doi: 10.1038/ni.3121.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#转录#
27
#Nat#
22
#Sox2#
31
#转录因子#
25