Clin Gastroenterol H:肝移植术后ABS患者金属支架的疗效及更佳持续时间如何?
2017-06-18 xing.T MedSci原创
由此可见,单次ERCP放置cSEMS的ABS的解决率似乎与多次ERCP放置PS的报道相当。支架插入时间越长,ABS解决率越高。
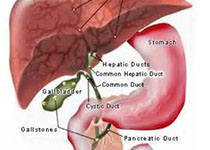
肝移植术后最常见的并发症之一是吻合口胆管狭窄(ABS)。内镜下逆行胰胆管造影(ERCP)插入塑料支架(PS)的做法在实现解决狭窄前往往需要多个程序才能完成。到目前为止,在ABS患者的治疗中采用覆膜自膨式金属支架(cSEMS)的研究报道了不同程度的疗效。近日,消化病领域权威杂志Clinical Gastroenterology and Hepatology发表了一篇研究文章,该研究的目的是分析ABS患者采用cSEMS治疗的长期疗效,并确定影响狭窄解决概率的因素。
研究人员通过内镜数据库查询确定了接受cSEMS治疗的ABS肝移植患者。研究人员分析了狭窄解决率、无狭窄间隔时间、狭窄解决的相关因素以及不良结局。
在44例肝移植且出现难治性ABS患者,这些患者接受了ERCP-cSEMS治疗,研究人员观察到33例患者狭窄得到解决(75%)。较长时间的cSEMS插入是与狭窄解决概率增加相关的唯一变量。cSEMS每增加一周,狭窄解决的几率增加20%。在33例初始狭窄解决的患者中,26例(78.8%)患者在整个随访期间保持胆管通畅。最常见的不良结局是cSEMS 发生内部的移位,其有11例患者(25%)发生这一不良结局。
由此可见,单次ERCP放置cSEMS的ABS的解决率似乎与多次ERCP放置PS的报道相当。支架插入时间越长,ABS解决率越高。
原始出处:
Sunguk Jang,et al. Efficacy and optimal duration of metallic stent in the management of refractory anastomotic stricture after liver transplantation. Clinical gastroenterology and hepatology 2017. http://www.cghjournal.org/article/S1542-3565(17)30721-8/fulltext
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#GAS#
45
#AST#
43
#移植术#
36
#Gastroenterol#
44
#金属支架#
44
学习了谢谢分享!!!
66
#持续时间#
37
学习啦!谢谢分享
63
学习了,谢谢作者分享!
76