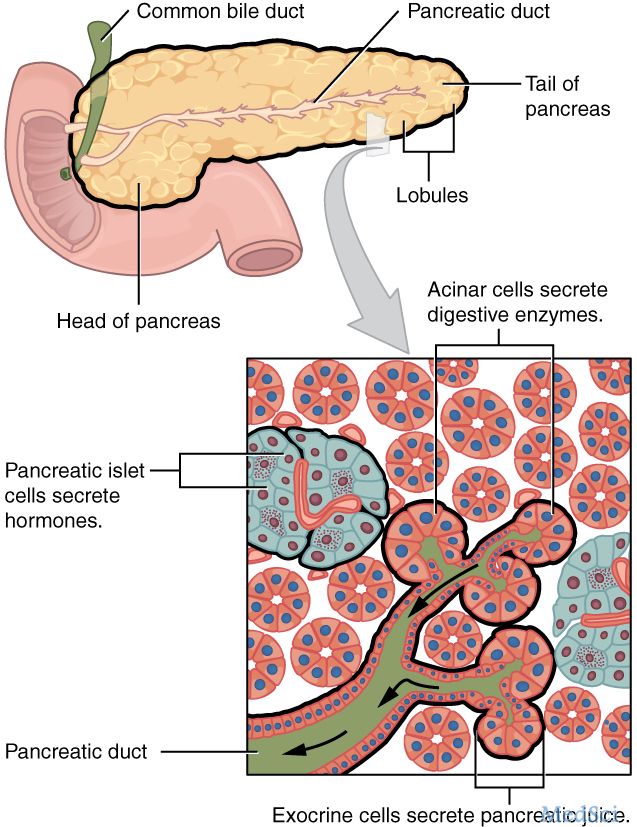
Lancet Gastroen Heptaol:紫杉醇+氟尿嘧啶:有望成为转移性胰腺癌的一线治疗
2017-03-21 高小羊 肿瘤时间
紫杉醇联合吉西他滨是转移性胰腺癌的标准治疗方案,然而回顾性资料显示 50%~60% 的患者对吉西他滨单药治疗无效,因此该方案并非最佳治疗方案。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#AST#
26
#Lancet#
26
#GAS#
30
希望有更多的循证证据支持
45
学习了分享了
58
学习了,分享了
42
#转移性#
29
#转移性胰腺癌#
35
#氟尿嘧啶#
27
感谢分享一下!
58