JCO:结直肠癌患者生存率预测新指标
2013-05-14 ecoliDH5 丁香园
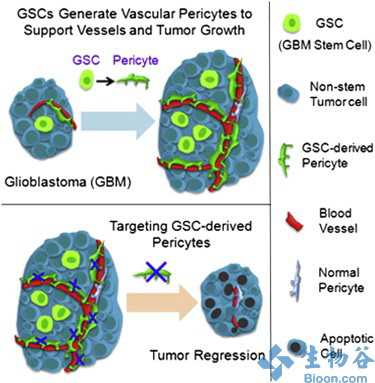
瘤体大小模型简图 通过TTG模型对OS的后验预测检验 A:西方患者;B:中国患者 在2013年5月6日在线出版的《临床肿瘤学杂志》(Journal of Clinical Oncology)上,发表了法国Pharsight咨询服务集团Rene Bruno博士等人的一项研究结果,该研究对新瘤体大小缓解指标在预测西方与中国结直肠癌(CRC)患者总生存率(OS)方面的应用进行评价。

瘤体大小模型简图

通过TTG模型对OS的后验预测检验
A:西方患者;B:中国患者
在2013年5月6日在线出版的《临床肿瘤学杂志》(Journal of Clinical Oncology)上,发表了法国Pharsight咨询服务集团Rene Bruno博士等人的一项研究结果,该研究对新瘤体大小缓解指标在预测西方与中国结直肠癌(CRC)患者总生存率(OS)方面的应用进行评价。
研究人员通过纵向比较瘤体大小相关模型,以及来自两项旨在对比考察贝伐单抗联合化疗方案与化疗方案用于一线治疗西方(n = 923)及中国(n = 203)CRC患者的临床III期研究,对各种瘤体大小缓解指标进行了估测。并通过预测OS的多变量模型,对基线预后因素及瘤体大小指标进行估测。通过对临床III期研究的多个副本进行模拟,评价相关模型的预测表现。
研究发现,对于OS预测,肿瘤生长时间(TTG)为最佳指标。TTG可完全捕获贝伐单抗效应。中国患者种群因素对OS或TTG-OS关系并无影响。模型可准确对各组OS分布情况以及贝伐单抗风险比进行预测(根据对西方患者观察,相关模型预测值, 0.75 v 0.68; 95%预测区间, 0.62至0.91)。
研究人员认为,对于接受贝伐单抗一线治疗的CRC患者,通过TTG参数可捕获到治疗获益。中国患者种群因素并无影响。因此,在早期临床研究数据的设计及分析中,对瘤体大小的数据纵向比较并基于模型的方式可作为一种有效手段。
与结直肠相关的拓展阅读:
- Sleep:睡眠过多或致结直肠癌风险升高
- Gut:常见遗传变异对结直肠癌风险具有累积影响
- Nature reviews:2012年结直肠癌研究的里程碑式突破
- 结直肠癌患者可在线申请慈善赠药---爱必妥
- J Clin Oncol:子宫内膜癌患者结直肠癌发生的风险多大? 更多信息请点击:有关结直肠更多资讯

Evaluation of Tumor-Size Response Metrics to Predict Overall Survival in Western and Chinese Patients With First-Line Metastatic Colorectal Cancer
Purpose
To assess new metrics of tumor-size response to predict overall survival (OS) in colorectal cancer (CRC) in Western and Chinese patients.
Patients and Methods
Various metrics of tumor-size response were estimated using longitudinal tumor size models and data from two phase III studies that compared bevacizumab plus chemotherapy versus chemotherapy as first-line therapy in Western (n = 923) and Chinese (n = 203) patients with CRC. Baseline prognostic factors and tumor-size metrics estimates were assessed in multivariate models to predict OS. Predictive performances of the models were assessed by simulating multiple replicas of the phase III studies.
Results
Time to tumor growth (TTG) was the best metric to predict OS. TTG fully captured bevacizumab effect. Chinese ethnicity had no impact on OS or on the TTG-OS relationships. The model correctly predicted OS distributions in each arm as well as bevacizumab hazard ratio (model prediction, 0.75 v 0.68 observed in Western patients; 95% prediction interval, 0.62 to 0.91).
Conclusion
TTG captured therapeutic benefit with bevacizumab in first-line CRC patients. Chinese ethnicity had no impact. Longitudinal tumor size data coupled with model-based approaches may offer a powerful alternative in the design and analysis of early clinical studies.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JCO#
22
#患者生存#
24
#生存率#
34
#结直肠#
23