塔斯玛尼亚恶魔,荒野中传播的癌症
2016-08-23 芦晓晶/赛先生 芦晓晶/赛先生
在今年7月14日出版的《Cell》杂志上,传染性癌症和分子进化领域著名学者,英国剑桥大学兽医系比较肿瘤学与遗传学准教授(编译者注:准教授(Reader),乃英国特色的教职,难以与大家熟悉的美国教职对应。在英国历史悠久的大学中,教授(Professor)职位很少,会在教授职级下面授予准教授教职,一般认为对应于美国的正教授或终身教职副教授。)Elizabeth P. Murchison 博士发
在今年7月14日出版的《Cell》杂志上,传染性癌症和分子进化领域著名学者,英国剑桥大学兽医系比较肿瘤学与遗传学准教授(编译者注:准教授(Reader),乃英国特色的教职,难以与大家熟悉的美国教职对应。在英国历史悠久的大学中,教授(Professor)职位很少,会在教授职级下面授予准教授教职,一般认为对应于美国的正教授或终身教职副教授。)Elizabeth P. Murchison 博士发表了一篇题为Cancer in the Wilderness,《荒野中的癌症》的文章,讲述了她在传染性癌症领域开展科学研究的心路历程。

图1. Elizabeth P. Murchison教授(图片来源:http://www.vet.cam.ac.uk/directory/murchison)
下面,笔者将追随Murchison的科研足迹,梳理一下 “可传染的癌症”这一领域的研究历史。
……当时,黑色的凤头鹦鹉在我头顶的林冠上尖叫着,我用手戳了戳那块肿瘤,并没有意识到,一场科学之旅即将展开,旅程环遍世界、穿越千年……
Elizabeth Murchison是澳大利亚人,一直到高中都生活在塔斯马尼亚;和大多数塔斯马尼亚年轻人一样,她高中毕业后离开了故乡的岛屿,去了墨尔本大学,专业是遗传学与生物化学。在墨尔本大学求学期间,Murchison受到 Mary-Jane Gething教授的影响,2002年大学毕业后选择到美国冷泉港实验室继续深造,攻读分子生物学与遗传学博士学位;博士学习期间Murchison的主要研究方向是当时新发现的RNA干扰现象的作用机制。就在Murchison在纽约求学期间,一种动物的命运在塔斯马尼亚引起了一丝波澜。
塔斯马尼亚恶魔面部肿瘤
塔斯马尼亚是一座心形的岛屿,陆地面积6.8万平方公里,位于澳大利亚大陆东南角约240公里的外海,是澳洲自然生态保护最完善的地区,全岛40%面积被正式列为国家公园、自然保护区或世界自然遗产[1]。作为与大陆隔离的独立岛屿,塔斯马尼亚拥有丰富而独特的动植物资源,袋獾是其中最具有代表性的物种之一。
袋獾(Sarcophilus harrisii)是塔斯马尼亚的特有物种,400年前在澳洲大陆绝迹,是20世纪30年代袋狼灭绝以后,地球上现存最大型的有袋类肉食动物,位于塔斯马尼亚食物链的最顶端。袋獾在野外寿命为5-6年,成年雄性体重可达7-13千克,雌性略小,一般与小狗的大小差不多,肌肉发达,咬合力强,昼伏夜出,以食腐为主。袋獾脾气暴躁,叫声尤其响亮刺耳,所以被本地人叫做“塔斯马尼亚恶魔(Tasmanian devil)”,并以这个名字着称于世。由于20世纪中叶以后的生态保护措施,袋獾的分布遍及塔斯马尼亚全岛,至90年代中期袋獾种群大小约为15万头[2,3]。

图2. 袋獾(塔斯马尼亚恶魔)的形象(图片来源:Wikipedia)

图3. 以塔斯马尼亚恶魔为原型的知名卡通角色Taz(图片来源:时代华纳)

图4. 以塔斯马尼亚恶魔为原型的吉祥物Tuz(装扮成linux吉祥物企鹅Tux的样子)(图片来源:Linux基金会)
1996年,在塔斯马尼亚岛东北角的国家公园,一只袋獾被发现罹患了一种头面部恶性肿瘤,这是这种疾病第一次被人们发现。其后,患有同样症状的个体不断被发现,它们通常在面部、口鼻周围出现恶性肿瘤,而且会很快发生全身转移,引起继发性感染,同时口腔肿瘤的持续生长会使病獾无法进食,最多六个月内就会造成患病个体死亡[4],这种疾病被命名为塔斯马尼亚恶魔面部肿瘤 (Tasmanian devil facial tumor disease, DFTD)。2001年以后,人们在更多的地域观察到了越来越多感染了DFTD的袋獾个体,而且在最初发现病患个体的地点附近,袋獾种群数量明显减少。这个现象引起了主管部门的重视,塔斯马尼亚第一产业与水利环境部 (DPIW) 组织了全境范围的普查,以评估DFTD对袋獾野外种群的影响[2]。

图5. 患DFTD的袋獾[5]
为应对DFTD,塔斯马尼亚第一产业与水利环境部于2003年成立了一个工作室进行数据整理与病理分析工作。2004年这个工作室被扩充成“恶魔疾病项目工作组 (Devil Disease Project Team)”,成员包括病理学家、生态学家及环保工作者[2]。2007年,主管部门基于这一工作组的研究结果制定了“恶魔岛计划 (The Devil Island Project, DIP)”,致力于重建袋獾种群。尽管人们作出了种种努力,DFTD的感染范围却越来越广,从被人们第一次发现之后的10年间,DFTD已经几乎传遍了布塔斯马尼亚全岛。受这种高致死性疾病影响,袋獾种群数量迅速下降,在最早发现DFTD的地区,至2006年袋獾数量下降了95%之多。按这种速度估算,袋獾在25-35年后将面临野外灭绝的危险[2,3]。2008年,国际自然保护联盟IUCN将袋獾列入了濒危物种红色名录。
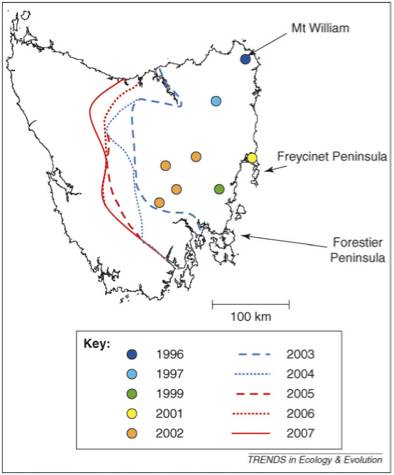
图6. DFTD的传播范围[3]
对DFTD的研究结果从2006年开始在国际期刊上陆续发表。行为学研究表明,袋獾间在争食、或更多的是在交配时,会互相撕咬,在头面部造成伤口,而肿瘤细胞也就有可能通过唾液、接触等方式直接接种在了原本健康的袋獾伤口中,并逐渐长大成为肿瘤。某种意义上,DFTD倒也可以被看做是一种性传播疾病,这也说明了为什么患DFTD的袋獾主要是两岁以上的性成熟个体[3]。
通过流行病学研究基本可以确定DFTD是一种传染性疾病,但其最初的发病来源并不清楚。某些病毒或细菌的感染是可能引发肿瘤的,比如在人体内,人类乳头瘤病毒(HPV)、乙肝病毒(HBV)、幽门螺杆菌(HP)等微生物的感染都可以促使特定癌症的发生。但是在DFTD患兽体内并没有检测出类似的微生物感染[4]。通过免疫组化等研究手段对DFTD肿瘤细胞进行组织学研究,鉴定出了表达于神经、表皮、内皮等组织的表面抗原,表明肿瘤可能原发自神经内分泌组织[6]。
在2006年发表于Nature杂志的一篇短篇通讯,使得人们对DFTD的关注扩展到了动物保护领域之外。DPIW的研究者通过细胞核型研究,确定了DFTD肿瘤细胞所发生的染色体缺失、重排等变异。最重要的发现是,虽然DFTD的肿瘤样本采集自生活在相距很远的不同地域的患病个体,但是所有样本中的肿瘤细胞全部具有相同的核型[7],说明所有患病袋獾身上的肿瘤细胞极有可能同属一个细胞系,具有相同的起源。更加通俗点讲, DFTD的癌细胞本身是能够相互传染的!
脱离了组织环境,动物细胞在自然环境中是很脆弱的,不能像细菌病毒等微生物那样可以通过空气、水、土壤等媒介进行宿主间转移。要实现细胞的异体转移,只能把细胞、组织直接从供体接种到受体,比如骨髓移植、输血等手术。更重要的一点,是动物本身的免疫系统会发现非自体组织并高效消灭之,外来的细胞在正常动物体内无法生存。因此,接受移植手术的患者需要长期使用免疫抑制剂,就是为了防止受体的免疫系统攻击移植的外源细胞和组织。
对DFTD肿瘤细胞组织相容性复合体(MHC)的研究不仅进一步证实了这些肿瘤细胞来源相同,更解释了这些外源肿瘤细胞为什么没有像在其他哺乳动物中一样被免疫系统所消灭[8]。MHC是一类位于细胞表面的蛋白分子,其氨基酸序列在同种动物的不同个体中具有多态性,也就是说不同个体间MHC分子具有特异性。除了参与免疫应答和调节,免疫系统是根据MHC的个体特异性来识别异体组织,引起排异反应的。进行器官移植手术之前需要做配型,就是为了筛选与受体MHC差异相对较小的合适供体,以降低排异反应的发生。袋獾种群中的遗传多态性,特别是MHC多态性很低,远低于人类及其他动物,使得袋獾的免疫系统不能有效识别、消灭来自于其他个体的肿瘤细胞,让外源肿瘤细胞得以存活、增殖,最终形成肿瘤并伺机侵染下一个目标[8-10]。
DFTD肿瘤可以通过癌细胞本身在动物个体之间传播,这种极不寻常的现象引起了很多遗传学家、肿瘤生物学家等研究者的广泛关注,这种传染性肿瘤成为肿瘤分子进化、群体遗传学、生态学等学科难得的研究对象。
对于DFTD的研究不仅有助于袋獾的保育,对其他濒危物种的保育也有借鉴意义。袋獾也可以作为自然选择压力下的行为学、物种演化等方面的研究对象——比如袋獾已经采取了更多“青春期性行为”等方式来应对种群数量的减少[11]。
当时仍然在冷泉港实验室攻读博士学位的Murchison对DFTD产生了浓厚的兴趣,这不仅是因为“传染性肿瘤”这种罕见的现象具有极大的研究价值,也因为她和塔斯马尼亚恶魔之间本就有着微妙的羁绊——由于塔斯马尼亚恶魔的卡通形象Taz传播甚广,这种代表性动物可能是世界其他地区的人们最(很可能是唯一)了解的有关塔斯马尼亚的事物。因此,作为冷泉港的“塔斯马尼亚女孩”,塔斯马尼亚恶魔常常成为Murchison在与同事交流时的引子与话题。
2006年1月,南半球的夏天,Murchison在塔斯马尼亚雨林的旅途中,第一次在路边见到了一只死于DFTD的年轻袋獾。就像篇首引语中描绘的那样,从此Murchison开始了她和塔斯马尼亚恶魔,和传染性癌症这一研究领域的不解之缘。
Murchison在冷泉港的博士导师,siRNA研究领域先驱之一的Greg Hannon教授,十分支持她把DFTD作为今后的研究方向。博士研究期间的训练使Murchison拥有了坚实的分子遗传学研究经验,当时正在兴起的第二代测序技术更使得对DFTD进行基因组水平的分析成为可能。Murchison 用来进行测序的第一个DFTD样本,正是来自她当年第一次在路边发现的塔斯马尼亚恶魔尸体。
离开美国后,Murchison在澳大利亚国立大学从事了一段短暂的研究工作,期间她通过转录组及microRNA测序,进一步确定了DFTD肿瘤细胞的单一来源——施万氏细胞(一种周围神经系统中的神经胶质细胞)[12]。
在2009年,由于澳大利亚NHMRC奖学金资助,Murchison获得了到著名的英国桑格研究院(Wellcome Trust Sanger Institute)开展博士后研究的机会,跟随癌症基因组领域著名学者Mike Stratton教授进行研究。通过基因组学分析不仅可以研究到底是哪些遗传性变异造成了DFTD,更可以此为契机进行癌症进化学研究。
2011年中,Murchison发表了以“与传染性癌症的斗争”为题的TED演讲。同月,两位澳大利亚DFTD研究者在《科学美国人》上发表了介绍塔斯马尼亚恶魔和DFTD的长篇文章[11]。通过大众科普媒体,传染性癌症第一次被民众大范围了解,这也成为一次对“恶魔岛计划”的成功推广,使得塔斯马尼亚恶魔的境遇受到了更广泛的关注。
2012年2月,Murchison对DFTD的基因组研究在Cell杂志上发表,这是人们第一次对传染性癌症进行基因组水平上的研究。该研究发现,所有的DFTD肿瘤细胞都可以追溯到一只雌性患病个体,在传播过程中,肿瘤细胞产生了约2万个遗传变异,这一数字与人类癌细胞在体内生长转移中产生的变异数目相当(在一个癌症病人体内的癌细胞亚克隆间可以观察到1千到3万个变异)。对大范围样本的测序结果,不仅支持和完善了之前对DFTD的遗传学、分子生物学研究,更可以系统的追踪肿瘤细胞在传播中产生的变异情况,建立癌细胞演化模型,对癌症遗传学和流行病学研究具有重要的参考意义[13]。接下来Murchison参与的一系列针对基因座、卫星序列、端粒等方面的研究进一步完善了这一模型[14-17]。
DFTD在袋獾个体间直接传播,是由于袋獾低水平的遗传多态性和MHC多态性。既然如此,那么是否存在其他的肿瘤细胞株也能够在袋獾种群间传播呢?答案是肯定的。2016年1月Murchison参与的一项最新研究,在塔斯马尼亚患病的袋獾种群中发现了一株与之前所观察到的DFTD在细胞形态、核型、基因序列特征上不同的肿瘤细胞。这种新发现的传染性袋獾肿瘤被称为DFT2[18]。DFT2的发现暗示了在袋獾种群中传染性肿瘤的发生几率要高于以往人们的估计,同时袋獾种群受到的疾病威胁也可能比以往的估计要严重得多,人们不能确定是否还有更多的尚未被发现的传染性肿瘤细胞株系存在于袋獾种群之中。
袋獾的遗传特点与生活习性造成了传染性肿瘤容易在种群内产生和传播,但是为什么直到1996年人们才发现这种现象,而在之前从未出现过?准确的原因我们不得而知。有可能是因为袋獾种群数量在之前的几个世纪中由于气候变化以及澳洲移民活动的影响而大幅度减少,从而大幅降低了袋獾种群的遗传多态性[19]。虽然20世纪后半叶袋獾种群数量得到了提高,但种群遗传多态性并没有同步恢复。由于这种高度遗传同质化的特点,加上较高的种群密度,使得肿瘤细胞通过某个偶然的契机——或许是某一次撕咬——开始在袋獾种群间肆虐。而DFTD造成的袋獾种群数量的迅速减小,更加剧了其种群遗传多态性的降低,形成了一个恶性循环。
DFTD作为一种存在了超过20年并不断发生突变的肿瘤细胞系,有没有可能随着突变的不断产生而在癌细胞基因组内积累足够的有害突变,最终自我消亡呢?这种情况似乎不太可能发生:如果将所有DFTD肿瘤细胞看做一个“种群”,“致死突变”的产生将随着突变细胞的死亡而消失,无法产生子代细胞,相当于被“自然选择”淘汰掉。
那么,袋獾未来的命运将如何?能否通过人工干预恢复野外种群?还是会逐步走向灭绝?我们现在不得而知。
由于被广泛研究和报道,DFTD作为一种传染性癌症而广受关注,但它其实并不是迄今为止唯一被人们发现的传染性肿瘤,而另一种比较温和的传染性肿瘤,不管是其被发现的历史,还是疾病产生发展的历史,都要比DFTD悠久得多。
犬传染性生殖器肿瘤
犬传染性生殖器肿瘤 (canine transmissible venereal tumor,CTVT),又称为Sticker氏肉瘤,是一种感染犬科动物的恶性肿瘤,通过交配、舔咬等方式在狗、狼等犬科动物间传播。CTVT传播范围广泛,在各大洲都有发现。早在1876年,人们就已经发现了CTVT这种传染性疾病,并通过实验证明了CTVT可以通过肿瘤细胞在犬间传染。20世纪80年代以来,CTVT逐渐被科学家用作癌症生物学的研究模型。
CTVT一般生长在阴茎基部或阴道前庭,早期表现为小而紧实的结节,晚期可生长为10cm直径额有蒂团块,通常伴有溃疡、渗液。尽管人们一般认为CTVT是恶性的,但是肿瘤细胞通常不会发生转移,也不会危及生命,有时病灶还会自行变小甚至消失[20]。
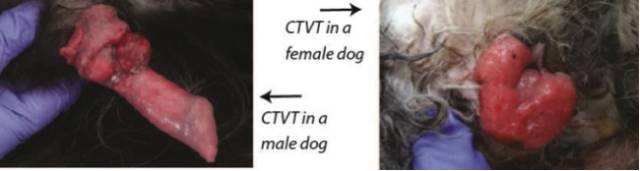
图7. CTVT病灶
对来自世界不同地区的CTVT样本进行核型分析,预示所有的CTVT肿瘤细胞很可能具有共同的来源,由于地理隔绝演化成为不同的亚群。1985年,科学家在来自于世界各地,分属不同进化亚群的CTVT样本中,发现了一个共同的独特遗传学特征,有力地支持了这个假说:在CTVT细胞中的Myc基因座位上插入了一个LINE元件(长散在重复序列),而这个特征在犬正常组织中是不存在的,这个遗传特征被作为了CTVT的诊断标准[21]。
2006年发表在Cell杂志上的一篇文章中,研究者检测了取自5个大洲的40条犬的CTVT细胞及正常组织。通过微卫星DNA、MHC、线粒体DNA检测,结果显示所有的CTVT都是进化同源的,与正常组织分属两个不同进化枝。不同来源的CTVT细胞间的遗传差异要小于CTVT细胞与宿主间的遗产差异[21],也就是说CTVT细胞是作为独立稳定的细胞系存在、传播与进化的。后来的其他独立研究也支持这一结论[22]。通过进化分析,CTVT产生的时间大概是在250到78000年前,可能来自于狼。不论CTVT实际产生于哪个年代,它都将是迄今已知的最古老的癌细胞系。
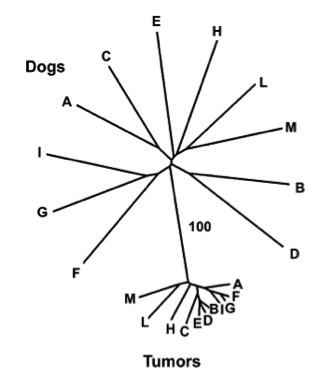
图8. CTVT与正常组织的微卫星序列进化树[21]
CTVT这一古老的疾病也是Murchison的研究兴趣之一。为了收集CTVT肿瘤样本,从地中海滨的意大利西西里峡谷,到非洲南端的佛得角海岸,再到安第斯山脉中的农场,Murchison的足迹遍及世界。与前人的研究结果一致,不管这些样本采集自世界哪一个角落,他们的遗传特征都说明:它们源自同一种细胞。
2013年,Murchison作为独立研究员受聘于剑桥大学,拥有了自己的实验室,继续从事传染性癌症研究。她在自己研究组的网页上向世界各地征集CTVT样本,网页上提供了指南,指导人们如何采集、保存、邮寄这些样本。
2014年,Murchison的研究组发表了关于CTVT基因组测序及分析的论文。研究分析数据显示CTVT肿瘤细胞的遗传相对稳定,同一个体内的CTVT细胞不像普通的人类癌细胞一样出现亚克隆分化。在CTVT细胞中观察到了大量的基因丢失,并鉴定出了多个CTVT遗传特征。通过对CTVT细胞、1000多条现代狗、以及多种犬科动物中的2万余个单核苷酸多态性位点比对,将CTVT产生的时间精确的定位在了距今11000年前,而其最初的宿主并非是之前研究推测的狼,而应该是一条类似于哈士奇的狗[23]。
在Murchison研究组刚刚发表的一篇论文中,研究人员对取自世界各地的四百多个CTVT样本的线粒体DNA进行了测序,发现这些传染性肿瘤细胞和他们的宿主间会发生线粒体DNA重组。通过进化分析,研究人员将来自不同地域的CTVT分为5个进化枝,这些结果不仅与它们的演化来源相符,也和近2000年来犬类随人类的迁徙历史相吻合。这个研究结果提示我们,线粒体DNA在肿瘤细胞的转移和癌症进化过程中,可能起到重要作用[24]。
自Murchison开始传染性癌症的研究以来,其持续不断的、有影响力的研究成果为她带来了包括“欧莱雅-联合国教科文组织青年女科学家(英国和爱尔兰)”和“英国癌症研究未来领袖”在内的诸多奖项和荣誉。
现在Murchison的研究方向依然聚焦在传染性癌症这一领域,与全世界的研究者一道,以DFTD、CTVT这两种仅有的哺乳动物传染性癌症作为研究对象,来进行癌细胞进化生物学研究,探寻这些肿瘤细胞是如何产生并适应他们的宿主,最终试图找寻治疗的方法。
在这篇小传的最后,Murchison写到:
今年初,我领着我的两个研究生去塔斯马尼亚南部进行野外考察。看着学生们开始着手解决他们自己的科学问题,不禁让我无比激动,这情景让我回想起当初在我选择这条不寻常的科研道路时,导师们给我的莫大支持与鼓励。我非常的幸运,有机会进入一个与众不同的重要领域,使我和我的故乡小岛独特的野生环境联系在一起。我非常幸运,邂逅了路边那只小小的野兽,改变了我的职业道路。(生物谷Bioon.com)
建议阅读
1.Ujvari, B., Papenfuss, A. T., and Belov, K. (2016)Transmissible cancers in an evolutionary context. Bioessays 38 Suppl 1, S14-23
2.Siddle, H. V., and Kaufman, J. (2015) Immunology of naturally transmissible tumours. Immunology 144, 11-20
3.Belov, K. (2012) Contagious cancer: lessons from the devil and the dog. Bioessays 34, 285-292
4.Jones, M. E., and McCallum, H. (2011) The devil's cancer. Scientific American 304, 72-77
5.Murchison,E. P. (2008) Clonally transmissible cancers in dogs and Tasmanian devils. Oncogene 27 Suppl 2, S19-30
参考文献
1. Tasmania wikipedia page.
2. Hawkins,C. E., Baars, C., Hesterman, H., Hocking, G.J., Jones, M.E., Lazenby, B., Mann,D., Mooney, N., Pemberton, D., Pyecroft, S., et al. (2006) Emerging disease and population decline of an island endemic, the Tasmanian devil Sarcophilus harrisii. Biological Conservation 131, 17
3. McCallum,H. (2008) Tasmanian devil facial tumour disease: lessons for conservation biology. Trends Ecol Evol 23, 631-637
4. Loh,R., Bergfeld, J., Hayes, D., O'Hara, A., Pyecroft, S., Raidal, S., and Sharpe,R. (2006) The pathology of devil facial tumor disease (DFTD) in Tasmanian Devils (Sarcophilus harrisii). Vet Pathol 43, 890-895
5. Jones,M. E., Cockburn, A., Hamede, R., Hawkins, C., Hesterman, H., Lachish, S., Mann,D., McCallum, H., and Pemberton, D. (2008) Life-history change indisease-ravaged Tasmanian devil populations. Proc Natl Acad Sci U S A 105,10023-10027
6. Loh,R., Hayes, D., Mahjoor, A., O'Hara, A., Pyecroft, S., and Raidal, S. (2006) The immunohistochemical characterization of devil facial tumor disease (DFTD) in the Tasmanian Devil (Sarcophilus harrisii). Vet Pathol 43, 896-903
7. Pearse,A. M., and Swift, K. (2006) Allograft theory: transmission of devilfacial-tumour disease. Nature 439, 549
8. Siddle,H. V., Kreiss, A., Eldridge, M. D., Noonan, E., Clarke, C. J., Pyecroft, S.,Woods, G. M., and Belov, K. (2007) Transmission of a fatal clonal tumor by biting occurs due to depleted MHC diversity in a threatened carnivorous marsupial. Proc Natl Acad Sci U S A 104, 16221-16226
9. Jones,M. E., Paetkau, D., Geffen, E., and Moritz, C. (2004) Genetic diversity and population structure of Tasmanian devils, the largest marsupial carnivore. Molecular ecology 13, 2197-2209
10. Siddle,H. V., Marzec, J., Cheng, Y., Jones, M., and Belov, K. (2010) MHC gene copy number variation in Tasmanian devils: implications for the spread of acontagious cancer. Proc Biol Sci 277, 2001-2006
11. Jones,M. E., and McCallum, H. (2011) The devil's cancer. Scientific American 304,72-77
12. Murchison,E. P., Tovar, C., Hsu, A., Bender, H. S., Kheradpour, P., Rebbeck, C. A.,Obendorf, D., Conlan, C., Bahlo, M., Blizzard, C. A., Pyecroft, S., Kreiss, A.,Kellis, M., Stark, A., Harkins, T. T., Marshall Graves, J. A., Woods, G. M.,Hannon, G. J., and Papenfuss, A. T. (2010) The Tasmanian devil transcriptome reveals Schwann cell origins of a clonally transmissible cancer. Science 327, 84-87
13. Murchison,E. P., Schulz-Trieglaff, O. B., Ning, Z., Alexandrov, L. B., Bauer, M. J., Fu,B., Hims, M., Ding, Z., Ivakhno, S., Stewart, C., Ng, B. L., Wong, W., Aken,B., White, S., Alsop, A., Becq, J., Bignell, G. R., Cheetham, R. K., Cheng, W.,Connor, T. R., Cox, A. J., Feng, Z. P., Gu, Y., Grocock, R. J., Harris, S. R.,Khrebtukova, I., Kingsbury, Z., Kowarsky, M., Kreiss, A., Luo, S., Marshall, J.,McBride, D. J., Murray, L., Pearse, A. M., Raine, K., Rasolonjatovo, I., Shaw,R., Tedder, P., Tregidgo, C., Vilella, A. J., Wedge, D. C., Woods, G. M.,Gormley, N., Humphray, S., Schroth, G., Smith, G., Hall, K., Searle, S. M.,Carter, N. P., Papenfuss, A. T., Futreal, P. A., Campbell, P. J., Yang, F.,Bentley, D. R., Evers, D. J., and Stratton, M. R. (2012) Genome sequencing and analysis of the Tasmanian devil and its transmissible cancer. Cell 148, 780-791
14. Deakin,J. E., Bender, H. S., Pearse, A. M., Rens, W., O'Brien, P. C., Ferguson-Smith,M. A., Cheng, Y., Morris, K., Taylor, R., Stuart, A., Belov, K., Amemiya, C.T., Murchison, E. P., Papenfuss, A. T., and Graves, J. A. (2012) Genomic restructuring in the Tasmanian devil facial tumour: chromosome painting and gene mapping provide clues to evolution of a transmissible tumour. PLoS Genet 8, e1002483
15. Nilsson,M. A., Janke, A., Murchison, E. P., Ning, Z., and Hallstrom, B. M. (2012)Expansion of CORE-SINEs in the genome of the Tasmanian devil. BMC Genomics 13, 172
16. Bender,H. S., Murchison, E. P., Pickett, H. A., Deakin, J. E., Strong, M. A., Conlan,C., McMillan, D. A., Neumann, A. A., Greider, C. W., Hannon, G. J., Reddel, R.R., and Graves, J. A. (2012) Extreme telomere length dimorphism in the Tasmanian devil and related marsupials suggests parental control of telomere length. PLoS One 7, e46195
17. Hamede,R. K., Pearse, A. M., Swift, K., Barmuta, L. A., Murchison, E. P., and Jones,M. E. (2015) Transmissible cancer in Tasmanian devils: localized lineage replacement and host population response. Proc Biol Sci 282
18. Pye,R. J., Pemberton, D., Tovar, C., Tubio, J. M., Dun, K. A., Fox, S., Darby, J.,Hayes, D., Knowles, G. W., Kreiss, A., Siddle, H. V., Swift, K., Lyons, A. B.,Murchison, E. P., and Woods, G. M. (2016) A second transmissible cancer in Tasmanian devils. Proc Natl Acad Sci U SA 113, 374-379
19. Bruniche-Olsen,A., Jones, M. E., Austin, J. J., Burridge, C. P., and Holland, B. R. (2014)Extensive population decline in the Tasmanian devil predates European settlement and devil facial tumour disease. Biology letters 10, 20140619
20. Murchison,E. P. (2008) Clonally transmissible cancers in dogs and Tasmanian devils. Oncogene 27 Suppl 2, S19-30
21. Murgia,C., Pritchard, J. K., Kim, S. Y., Fassati, A., and Weiss, R. A. (2006) Clonalorigin and evolution of a transmissible cancer. Cell 126, 477-487
22. Rebbeck,C. A., Thomas, R., Breen, M., Leroi, A. M., and Burt, A. (2009) Origins and evolution of a transmissible cancer. Evolution;international journal of organic evolution 63, 2340-2349
23. Murchison,E. P., Wedge, D. C., Alexandrov, L. B., Fu, B., Martincorena, I., Ning, Z.,Tubio, J. M., Werner, E. I., Allen, J., De Nardi, A. B., Donelan, E. M.,Marino, G., Fassati, A., Campbell, P. J., Yang, F., Burt, A., Weiss, R. A., and Stratton, M. R. (2014) Transmissible [corrected] dog cancer genome reveals the origin and history of an ancient cell lineage. Science 343, 437-440
24. Strakova,A., Ni Leathlobhair, M., Wang, G. D., Yin, T. T., Airikkala-Otter, I., Allen,J. L., Allum, K. M., Bansse-Issa, L., Bisson, J. L., Castillo Domracheva, A.,de Castro, K. F., Corrigan, A. M., Cran, H. R., Crawford, J. T., Cutter, S. M.,Delgadillo Keenan, L., Donelan, E. M., Faramade, I. A., Flores Reynoso, E.,Fotopoulou, E., Fruean, S. N., Gallardo-Arrieta, F., Glebova, O., Hafelin Manrique,R. F., Henriques, J. J., Ignatenko, N., Koenig, D., Lanza-Perea, M., Lobetti,R., Lopez Quintana, A. M., Losfelt, T., Marino, G., Martincorena, I., Martinez Castaneda, S., Martinez-Lopez, M. F., Meyer, M., Nakanwagi, B., De Nardi, A.B., Neunzig, W., Nixon, S. J., Onsare, M. M., Ortega-Pacheco, A., Peleteiro, M.C., Pye, R. J., Reece, J. F., Rojas Gutierrez, J., Sadia, H., Schmeling, S. K.,Shamanova, O., Ssuna, R. K., Steenland-Smit, A. E., Svitich, A., Thoya Ngoka,I., Vitalaru, B. A., de Vos, A. P., de Vos, J. P., Walkinton, O., Wedge, D. C.,Wehrle-Martinez, A. S., van der Wel, M. G., Widdowson, S. A., and Murchison, E.P. (2016) Mitochondrial genetic diversity, selection and recombination in acanine transmissible cancer. Elife 5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













很好,不错,以后会多学习
76
继续学习
62
继续关注
63
很好的研究课题!学习了!!
67
阅读了。
61
值得学习
27
谢谢,学习了
27
学习学习!
37
厉害,高大上的研究
32
学习起来
22