Cell Rep:不同肿瘤细胞可相互协作促进恶性黑色素瘤的扩散
2014-07-28 佚名 生物谷
近日,刊登在国际杂志Cell Reports上的一篇研究论文中,来自曼彻斯特大学的研究人员表示,皮肤癌细胞可以互相合作实现在机体中的快速扩散,某些黑色素瘤细胞生长速度尤其之快,但这些癌细胞却并不擅长于侵袭周围的组织,而其它黑色素瘤细胞则完全相反,它们虽然生长缓慢但是可以快速实现周围组织的侵袭,相关研究为开发新型药物来治疗黑色素瘤提供了一定帮助。在肿瘤组织中一种名为捎带细胞(Piggy-backin
近日,刊登在国际杂志Cell Reports上的一篇研究论文中,来自曼彻斯特大学的研究人员表示,皮肤癌细胞可以互相合作实现在机体中的快速扩散,某些黑色素瘤细胞生长速度尤其之快,但这些癌细胞却并不擅长于侵袭周围的组织,而其它黑色素瘤细胞则完全相反,它们虽然生长缓慢但是可以快速实现周围组织的侵袭,相关研究为开发新型药物来治疗黑色素瘤提供了一定帮助。
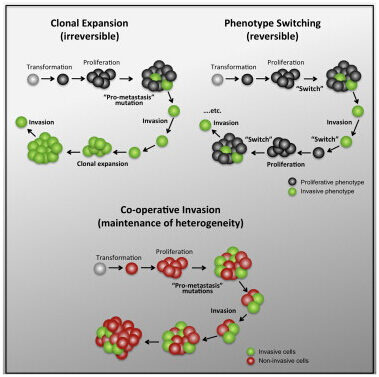
在肿瘤组织中一种名为捎带细胞(Piggy-backing cells)的快速生长的细胞往往会同高度侵袭性的细胞一起,一旦其到达机体的不同部位就会开启高效的侵袭模式,最终形成新的肿瘤组织。文章中研究者利用透明斑马鱼进行研究,以便其可以观察到癌细胞如何在机体中移动以及如何进行侵袭。
研究者Claudia Wellbrock表示,过去我们常常认为癌细胞是通过特异性侵袭到机体其它组织中来进行扩散,但是本文研究中我们却发现黑色素瘤细胞可以通过互相合作的侵袭模式来进行扩散;不同类型的癌细胞可以同时在肿瘤组织中存在,而且可以通过互相协作来进行高效扩散,这对于后期我们开发治疗性的策略往往具有一定的指示意义。
黑色素瘤是一种恶性的皮肤癌,在英国每年大约有1.33万人被诊断患有该疾病;而令人比较担忧的是近些年来恶性黑色素瘤的发病率相比20世纪70年代增加了超过5倍;研究者Richard Marais教授说道,恶性黑色素瘤是一种恶性的皮肤癌,其通常可以快速扩散并且引发恶性病变,这项研究就揭示了恶性黑色素瘤高效快速扩散的分子机制;近些年来随着恶性黑色素瘤有效疗法的开发,相信在不久的将来我们就可以成功治疗该疾病,当然平时我们也需要加强早期黑色素瘤的诊断,以早日预防黑色素瘤的产生。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CEL#
25
#色素#
34
#Cell#
27
#肿瘤细胞#
27
#黑色素#
33
#黑色素#
27