NEJM:达雷木单抗联合疗法有助于改善新诊断AL淀粉样患者预后
2021-07-04 MedSci原创 MedSci原创
新诊断AL淀粉样患者,在硼替佐米、环磷酰胺和地塞米松联合治疗基础上添加CD38达雷木单抗有助于提高患者血液学完全应答率,降低主要器官恶化或血液学进展风险
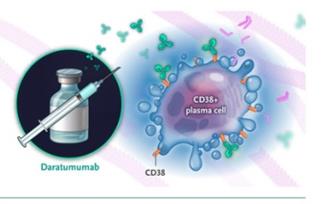
免疫球蛋白轻链型(AL)淀粉样变是一种克隆性、非增殖性浆细胞疾病,其免疫球蛋白可沉积于不同的组织部位或器官中,并导致一系列症状,如限制性心肌病、肾病综合征、肝衰竭、周围/自主神经病及无症状性多发性骨髓瘤等,CD38+浆细胞的克隆性扩增是重要的发病机制。目前标准治疗方案为使用多发性骨髓瘤衍生的靶向血浆细胞疗法--即硼替佐米、环磷酰胺和地塞米松联合治疗。达雷木单抗(Daratumumab)是一种CD38靶向抗体,目前用于接受过三次以上治疗(包括蛋白酶抑制剂、免疫调节剂和两者联用)的多发性骨髓瘤患者的治疗。近日研究人员考察了其对新诊断AL淀粉样病患者的临床效果。
新诊断的AL淀粉样病患者参与研究,在6轮的硼替佐米-环磷酰米-地塞米松联合治疗基础上,随机接受安慰剂或达雷木单抗治疗,达雷木单抗组每4周进行一次皮下注射,持续最多24轮。研究的主要终点是血液学完全应答。
共有388例患者参与研究,平均随访时间11.4个月。达雷木单抗组血液学完全应答率显著高于对照组(53.3% vs 18.1%,相对风险比=2.9)。达雷木单抗组在无主要器官恶化或无血液学进展生存率方面有优势(主要器官恶化、血液学进展或死亡的危险比为0.58)。6个月时,达雷木单抗组心脏(41.5% vs 22.2%)和肾(53.0% vs 23.9%)治疗应答率高于对照组。最常见的3级或4级不良事件是淋巴细胞减少(达雷木单抗组vs 对照组=13.0% vs 10.1%)、肺炎(7.8% vs 4.3%)、心力衰竭(6.2% vs 4.8%)和腹泻(5.7% vs 3.7%)。达雷木单抗组7.3%的患者出现药物相关的系统性反应。共有56例患者死亡(达雷木单抗组27例,对照组29例),大多数死于淀粉样病相关心肌病。

组间无主要器官恶化或无血液学进展生存率差异
研究认为,对于新诊断AL淀粉样患者,在硼替佐米、环磷酰胺和地塞米松联合治疗基础上添加CD38达雷木单抗有助于提高患者血液学完全应答率,降低主要器官恶化或血液学进展风险。
原始出处:
Efstathios Kastritis et al. Daratumumab-Based Treatment for Immunoglobulin Light-Chain Amyloidosis. N Engl J Med,July 01,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









达雷妥尤单抗?
40
#新诊断#
28
#联合疗法#
37
#患者预后#
25
理学原子核
56
#达雷木单抗#
34
已读,真是受益匪浅。
60
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
41