Neurology CP:心脏骤停和胸外按压期间的脑电图改变
2018-07-17 杨中华 脑血管病及重症文献导读
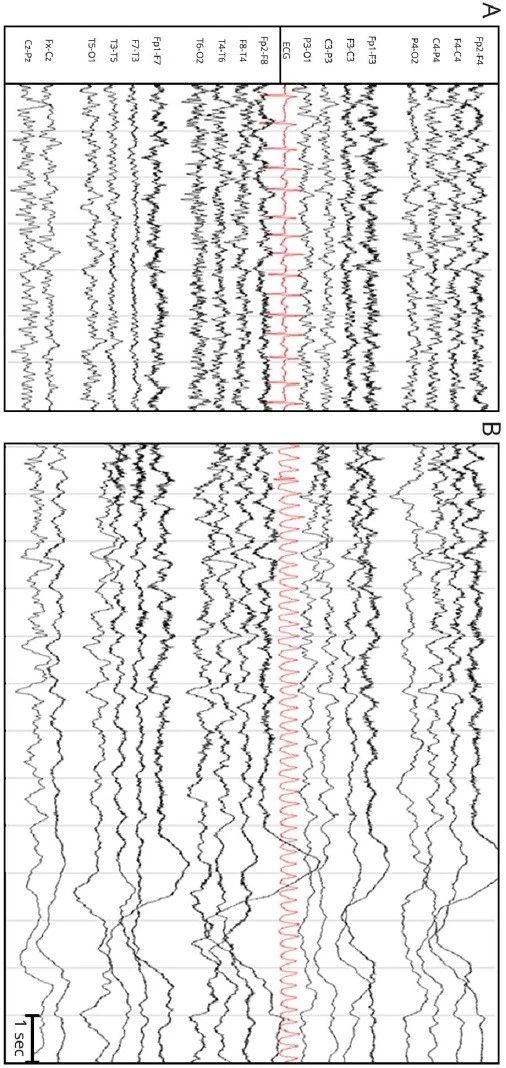
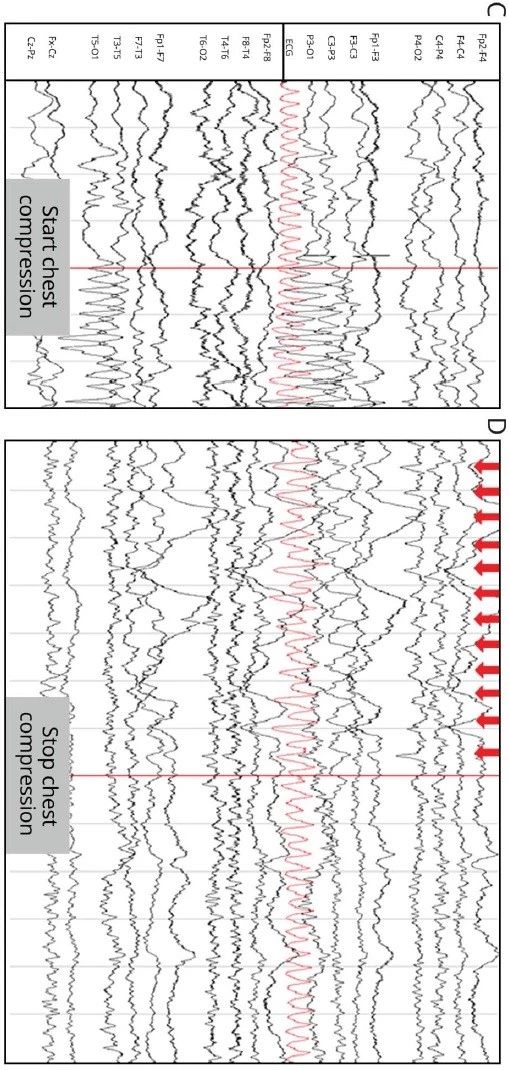
在进行21导脑电图(EEG)检测时突发室性心动过速(VT)。VT 40秒后EEG记录到高频电活动(higher frequency elements)波幅降低,以前有人认为这个现象发生于心脏停跳30秒以内。胸外按压几秒钟后EEG活动恢复,提示脑灌注增加。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#按压#
72
#Neurol#
33
#胸外按压#
39
好文献学习了
49
好
70