Cell:肠道菌研究新工具
2017-04-24 佚名 生物探索
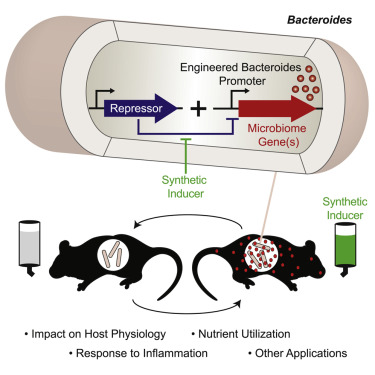
在4月21日的Cell上,有两篇文章在单细胞和基因基础上提供了改进的遗传工具,用于剖析细菌群落的空间组织和时间动态。可调启动子的工程菌植入小鼠,可以区分单个细胞菌株的表达状况。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CEL#
26
#Cell#
27
学习了,谢谢分享
53
文章很好,拜读了
49
学习了分享了谢谢!
48
学习了,谢谢分享
52
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。给点赞啦……
52
学习了,谢谢分享
21
#肠道菌#
22
学习一下觉得非常好
21