立体定向活检诊断双侧岛叶恶性囊性病变1例
2019-08-29 张环 姜俊男 郭志钢 中国实验诊断学
患者:女,35岁,因左侧肢体及左侧颜面部间断性麻木6个月伴头痛,于2005年10月到我院就诊。患者入院前1个月在其他医院行头部MRI检查后发现颅内占位病变。患者发病后,无发热,无体重减轻,无抽搐。入院后查体:意识清,双瞳等大同圆,瞳孔直径2.0mm、对光反射灵敏,言语应答准确,左侧上、下肢肌力Ⅳ级,右侧上、下肢肌力Ⅴ级,无病理反射。
1.病例资料
患者:女,35岁,因左侧肢体及左侧颜面部间断性麻木6个月伴头痛,于2005年10月到我院就诊。患者入院前1个月在其他医院行头部MRI检查后发现颅内占位病变。患者发病后,无发热,无体重减轻,无抽搐。入院后查体:意识清,双瞳等大同圆,瞳孔直径2.0mm、对光反射灵敏,言语应答准确,左侧上、下肢肌力Ⅳ级,右侧上、下肢肌力Ⅴ级,无病理反射。
患者头部MRI平扫及增强扫描显示:双侧岛叶可见两处类圆形T1不均匀信号、T2高信号影,左右两侧病灶大小分别为:21mm×20mm×28mm和23mm×22mm×27mm,两处病灶增强后均显示边界清晰的环形强化影,右侧病变内有明显分隔,左侧病变内部组织有点状强化影,两侧病灶周边均可见明显水肿带(图1A)。
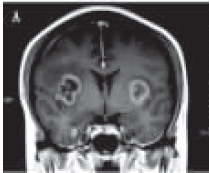
图1A:冠状位MRI增强图像显示双侧岛叶两处类圆形异常信号影,边界均呈环形强化,右侧病变内有明显分隔,两侧病灶周边均可见明显水肿带;
根据病史、查体及影像学检查结果,考虑患者病灶性质可能为恶性肿瘤(胶质瘤、恶性脑膜瘤、脑转移瘤)或脑脓肿。患者入院后其他脏器检查未发现占位病变。患者入院后第4日,应用CT定位立体定向仪(Komai's CT-Stereotactic Frame)行立体定向颅内占位病变活检诊断手术。术中于左侧额部单孔钻颅,立体定向穿刺针进入病灶中心靶点,分2次抽出黄色、不透明液体共5.5ml,液体中可见少许白色粒状物。
立体定向穿刺针后退1.0 cm,以螺旋活检针取材出灰白色、质韧状囊壁组织,大小为1.0mm×3.0mm。术后穿刺液细胞学检查镜下见到少量核大小、形态异常,核染色质增多,分布不均,核膜增厚,边界不整齐的核异质改变细胞。术后病理检查,HE染色显示见到恶性肿瘤细胞(图1B)。病理检查结果经北京协和医院病理科刘彤华院士会诊,认为可以诊断为颅内恶性囊性病变,但因病灶囊壁处活检取材组织体积小,不能确切判定出病变的具体种类。随访证实患者于手术后1个月死亡。

图1B:病变囊壁组织病理HE染色显示见到恶性肿瘤细胞,×100。
2.讨论
立体定向活检手术是诊断颅内复杂病变的重要方法。随着立体定向设备和影像学技术的不断进步,立体定向活检手术从以前的有框CT和有框MRI定位,又发展到无框CT定位和无框MRI定位及神经导航定位等多种手术方法。虽然无框的立体定向手术会减少患者的痛苦,但大宗病例的回顾性研究表明:有框的CT定位立体定向手术具有更好的取材准确性。
本例患者为双侧岛叶囊性占位病变,且囊壁组织较薄,因而对活检取材部位的选取要求更高。氢质子磁共振波谱引导立体定向活检手术,对于病灶实体体积较大的病变具有取材位置的指导意义。对于囊性病变的立体定向活检手术,单纯的囊壁组织的立体定向靶点定位更为重要。从本例患者的影像学MRI及MRI增强图像分析,患者的右侧病灶周边强化较均匀、内部有明显分隔、病灶周边水肿范围较大,考虑脑脓肿的可能性偏大。而患者的左侧病变周边不但存在强化影且内部组织也有点状强化影,病灶周边水肿范围较小,考虑左侧病灶为恶性的可能性较大。
更为重要的是,MRI增强图像显示左侧病灶囊壁相对较厚,活检诊断成功的概率要大于右侧病灶。因而,我们的活检手术选取了患者的左侧病灶。我们在立体定向活检手术中,抽吸出5.5ml囊液,且囊液中含部分实体组织,又成功的取出了部分囊壁组织。术后穿刺液细胞学检查及术后囊壁组织病理学检查均见到恶性肿瘤细胞。
本例患者的病理检查结果经北京协和医院病理科刘彤华院士会诊,虽然不能确切判定出病变的具体种类,但因囊壁组织中见到了恶性肿瘤细胞,可以诊断为颅内恶性囊性病变。患者的随访结果,也与颅内恶性病变的预后相符。依据本例手术的经验和体会,我们在其他患者的颅内囊性病变的立体定向活检诊断中,相继成功的完成了脑干囊性胶质瘤和脑干囊性转移癌(源于肺鳞腺癌)的诊断。总之,立体定向活检手术对于颅内复杂的囊性疾病的诊断具有重要意义,手术成功的关键在于能否在活检手术过程中准确取到病变的囊壁组织。
原始出处:
张环,姜俊男,郭志钢, 等.立体定向活检诊断双侧岛叶恶性囊性病变1例[J].中国实验诊断学,2018,(7):1273-1274.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#立体定向活检#
45
#定向#
27
#囊性#
37
#立体定向#
37
#活检#
38
#双侧#
25