Oncotarget:石胆酸能杀死癌细胞但不伤害健康细胞
2012-01-06 MedSci原创 MedSci原创
(LCA抗肿瘤的机制模型:a. 细胞系BE(2)-m17. b. 细胞系SK-n-MCIXC) 2012年1月4日,据《每日科学》报道,在消化过程中由肝脏自然产生,其作用已被严重低估。发表在Oncotarget期刊上的一项研究表明,LCA可以杀死数种类型的癌细胞,如那些发现于脑肿瘤和乳腺癌中的癌细胞。 该研究小组,由Concordia大学领导,同时包括来自麦吉尔大学、蒙特利尔犹太总医院戴维斯研
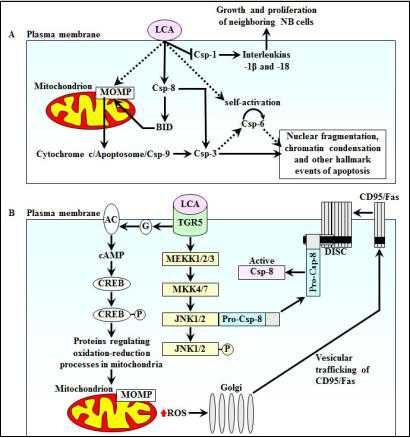
(LCA抗肿瘤的机制模型:a. 细胞系BE(2)-m17. b. 细胞系SK-n-MCIXC)
2012年1月4日,据《每日科学》报道,在消化过程中由肝脏自然产生,其作用已被严重低估。发表在Oncotarget期刊上的一项研究表明,LCA可以杀死数种类型的癌细胞,如那些发现于脑肿瘤和乳腺癌中的癌细胞。
该研究小组,由Concordia大学领导,同时包括来自麦吉尔大学、蒙特利尔犹太总医院戴维斯研究所及Saskatchewan大学的科学家。
这个团队以前的研究表明,LCA可以延长老化酵母的生命周期。这一次,该研究小组发现LCA具有非常强的选择性地杀死癌细胞,同时对正常细胞毫发无损。这可能预示着化疗药物的一个巨大的进步。
"LCA不仅能杀死癌细胞,也可以防止整个肿瘤的生长,"通讯作者Vladimir Titorenko说,生物系教授及Concordia大学基因组学、细胞生物学和老化的研究主席。
更重要的是,LCA能够阻止肿瘤释放出引起邻近癌细胞生长和增殖的物质。 Titorenko说LCA是唯一的靶向肿瘤细胞的化合物,可以转化为终止-肿瘤的力量。
"防止癌细胞扩散到身体的其他部位,这是非常重要的,"他说,不像其他的抗衰老化合物,LCA能终止癌细胞的生长,但仍让正常细胞继续生长。
在不同类型癌症中的广泛作用
研究小组下一步将在小鼠模型中测试LCA对不同癌症的效果。 Titorenko期望,LCA也能够杀死这些实验中的癌细胞,并最终走向人体临床试验。 "我们的研究发现,LCA不仅能杀死肿瘤(神经母细胞瘤),也可以杀死人类乳腺癌细胞,"Titorenko说。 "这表明,它对不同类型的癌症有广泛的作用。"
Titorenko强调,与化疗所用药物不同,LCA是一种天然化合物,已经存在于我们的体内。有研究表明,LCA可以通过添加到食物中由小鼠安全的摄取。那么为什么LCA对癌细胞是致命的?Titorenko推测,癌细胞有更多的LCA感受器,这使得它们比正常细胞对化合物更敏感。
LCA感受器发出信号至线粒体--所有细胞的能量工厂。似乎当这些信号过强时,线粒体就会自毁,随之整个细胞崩解。简而言之,Titorenko和他的同事们正致力于研究通过癌细胞对LCA的一个弱点来破坏癌细胞。
这一研究得到了加拿大卫生研究院、加拿大自然科学和工程研究理事会、Concordia大学研究讲座计划的资助。(生物谷bioon.com)

PMID:21992775
Lithocholic bile acid selectively kills neuroblastoma cells, while sparing normal neuronal cells
Goldberg AA, Beach A, Davies GF, Harkness TA, Leblanc A, Titorenko VI
Abstract: Aging is one of the major risk factors of cancer. The onset of cancer can be postponed by pharmacological and dietary anti-aging interventions. We recently found in yeast cellular models of aging that lithocholic acid (LCA) extends longevity. Here we show that, at concentrations that are not cytotoxic to primary cultures of human neurons, LCA kills the neuroblastoma (NB) cell lines BE(2)-m17, SK-n-SH, SK-n-MCIXC and Lan-1. In BE(2)-m17, SK-n-SH and SK-n-MCIXC cells, the LCA anti-tumor effect is due to apoptotic cell death. In contrast, the LCA-triggered death of Lan-1 cells is not caused by apoptosis. While low concentrations of LCA sensitize BE(2)-m17 and SK-n-MCIXC cells to hydrogen peroxide-induced apoptotic cell death controlled by mitochondria, these LCA concentrations make primary cultures of human neurons resistant to such a form of cell death. LCA kills BE(2)-m17 and SK-n-MCIXC cell lines by triggering not only the intrinsic (mitochondrial) apoptotic cell death pathway driven by mitochondrial outer membrane permeabilization and initiator caspase-9 activation, but also the extrinsic (death receptor) pathway of apoptosis involving activation of the initiator caspase-8. Based on these data, we propose a mechanism underlying a potent and selective anti-tumor effect of LCA in cultured human NB cells. Moreover, our finding that LCA kills cultured human breast cancer and rat glioma cells implies that it has a broad anti-tumor effect on cancer cells derived from different tissues and organisms.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#target#
40
#癌细胞#
27
#健康细胞#
36