BMJ:肺栓塞驼峰征-案例报道
2016-05-09 Mechront 译 MedSci原创
患者女,60岁,急性胸膜炎性胸痛和呼吸困难就诊,不伴咳痰。病程期间患者经历了不适、间歇热、寒颤4周。10年前患者心脏听证闻及杂音,经胸超声心动图检查后,诊断为动脉导管未闭(PDA)。入院时,患者体温39°C;左侧胸膜摩擦感;前胸导联有机械杂音;心电图未见明显异常;查血提示正常红细胞性贫血、白细胞增多、肾功未见明显异常;三份血液培养均显示B组链球菌;胸片结果如下图:1-患者的胸片结果有什么异常,
患者女,60岁,急性胸膜炎性胸痛和呼吸困难就诊,不伴咳痰。病程期间患者经历了不适、间歇热、寒颤4周。
10年前患者心脏听证闻及杂音,经胸超声心动图检查后,诊断为动脉导管未闭(PDA)。
入院时,患者体温39°C;左侧胸膜摩擦感;前胸导联有机械杂音;心电图未见明显异常;查血提示正常红细胞性贫血、白细胞增多、肾功未见明显异常;三份血液培养均显示B组链球菌;胸片结果如下图: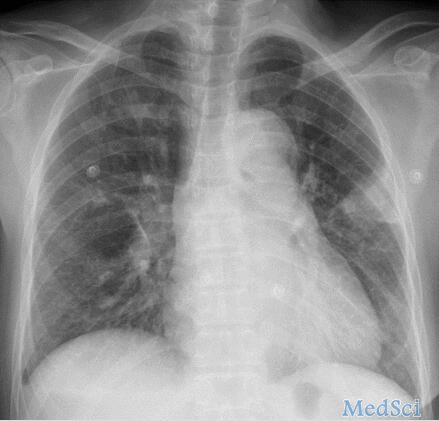
1-患者的胸片结果有什么异常,与胸膜摩擦有什么关系?
如下图“叉叉”所示区域,患者的左肺有一块三角形(楔形)阴影,对应临床病史胸痛和查体时胸膜摩擦区域。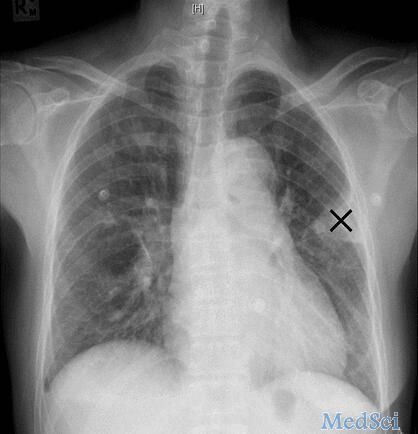
该区域的表现成为“Hampton's hump 征”(驼峰征),在1940年由Hampton 和 Castleman 首次提出。X线主要表现为肺外周邻近胸膜的楔形磨玻璃样阴影,峰尖与肺动脉末梢部相连,为肺动脉末梢部梗塞所产生的肺梗塞,标志着肺栓塞远端的肺已发生梗死,可与肺炎阴影鉴别。
2-考虑到患者的临床表现和既往PDA病史,导致异常的原因最可能原因是什么?
感染性心内膜炎是先天性心脏病罕见但十分重要的并发症。患者的胸膜炎胸痛表现和胸片影像学改变符合肺炎或肺栓塞(肺梗死)。
本案例中的患者有PDA病史,现有感染性心内膜炎证据(发热寒颤症状和培养证实B组链球菌败血症;此外,病程期间患者还出现过紫癜样皮疹,结合发热和寒颤,提示血管炎),加之临床表现和影像学证据,需要考虑肺感染性肺栓塞。
动脉导管原本系胎儿时期肺动脉与主动脉间的正常血流通道,由于此时肺呼吸功能障碍,来自右心室的肺动脉血经导管进入降主动脉,而左心室的血液则进入升主动脉,故动脉导管为胚胎时期特殊循环方式所必需。出生后,肺膨胀并承担气体交换功能,肺循环和体循环各司其职,不久导管因废用即自选闭合。如持续不闭合而形成PDA。PDA是较常见的先天性心血管畸形,占先天性心脏病总数的10%左右。
PDA患者并发感染性心内膜炎,感染性赘生物通常发生于动脉导管的肺动脉端,所以栓塞事件通常发生在肺部而不是全身血液循环。
随着外科手术修补技术和抗生素的广泛使用,目前英国PDA并发内膜炎的年发病率低于0.45-1%。
3-如何确诊?
可疑肺栓塞患者需要进一步的影像学检查。D-二聚体可以作为排除诊断标准之一,肺通气/灌注显像对慢性栓塞性肺动脉栓子的检测更为敏感,在这种情况下,CT肺血管造影(CTPA)更有用,可以更好的诊断急性左侧肺栓塞与肺梗死。CTPA对于急性肺栓塞高危患者而言,是一种快速、准确、灵敏的一线影像学检查。
CTPA检查结果如下图所示,红色箭头为左肺动脉,其内有肺栓塞,黄色箭头为远端肺梗死,与胸片区域一致,紫色箭头为钙化的PDA,位于主动脉弓和肺动脉之间。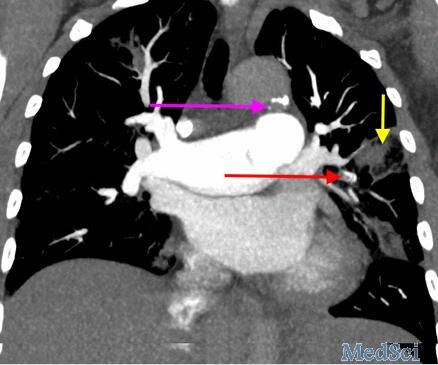
4-心脏成像技术选择什么?
可疑感染性心内膜炎时,首选超声心动图,可以评估右心瓣膜及相关瓣膜功能障碍的严重程度。本例患者的超声心动图检查结果如下图所示,肺动脉瓣水平左室短轴经胸超声心动图显示赘生物(黄色箭头)位于升主动脉(红色箭头)旁的肺动脉主干(蓝色箭头)内。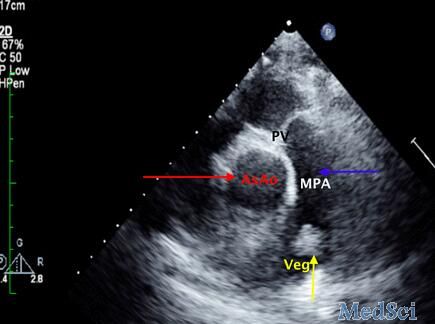
超声心动图彩色多普勒血流信号提示血液从主动脉弓返流入肺动脉,证实PDA。
5-治疗
目前患者的诊断有肺栓塞、PDA、感染性心内膜炎。对患者进行心胸手术,封闭PDA,切除赘生物。患者的病情很复杂,因为她还出现了播散性感染如化脓性膝关节炎(需要关节冲洗)和颈椎椎间盘炎。在完全康复前,需要静脉注射抗生素6周。
附:感染性心内膜炎Duke诊断标准:
确定诊断: 2条主要标准或1条主要标准+3条次要标准或5条次要标准。
可能诊断:1条主要标准+1条次要标准;或3条次要标准。
主要标准:
(1)血培养阳性:两次不同的血培养均为IE的典型致病菌(草绿色链球菌、牛链球菌、HACEK组细菌、金黄色葡萄球菌或社区获得性肠球菌而无原发病灶);或非上述细菌但与IE一致的微生物持续性血培养阳性(持续性阳性定义为相隔>12小时的2次或2次以上血培养阳性;或首末次血培养相隔时间>1小时的3次血培养全部阳性、4次全部阳性)。
(2)单次血培养阳性为贝氏柯克斯体或I期IgG滴度>1:800。
(3)超声心动图发现感染性心内膜炎的阳性表现:①赘生物,②心脏脓肿,③新发生的人工瓣膜裂开。
(4)新发生的瓣膜返流。
次要标准:
(1)易患因素、基础心脏病或静脉吸毒成瘾。
(2)体温>38℃的发热。
(3)血管损害征象:大动脉栓塞,脓毒栓塞性肺梗死,霉菌性动脉瘤、颅内出血、结膜出血、Janeway损伤等。
(4)免疫异常征象:肾小球肾炎、Osler结节、Roth出血点及类风湿因子。
(5)微生物学证据:血培养阳性但未能达到主要标准要求;或与感染性心内膜炎一致的活动性细菌感染的血清学证据。
原始出处:
Tom Ford,David Rees, Patent ductus arteriosus illuminating an old eponym.BMJ 2016; 353 doi: http://dx.doi.org/10.1136/bmj.i2182 (Published 06 May 2016)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#BMJ#
25
不错哦继续关注
75
关注值得学习。赞!好文有待探究。
75
深入学习,好文值得点赞!
80
值得学习
110
感觉在临床上不多见
94
值得阅读,学习!
137
扩展知识范围
76