Cell Death Dis:AMPK激动剂通过激活高脂和链脲佐菌素诱导的糖尿病小鼠的自噬来缓解肾小管间质纤维化。
2021-10-17 从医路漫漫 MedSci原创
糖尿病肾病(DN)是糖尿病患者最严重的微血管并发症之一。大约30-40%的糖尿病(DM)患者发展为肾病并进展为肾损伤。它显著降低了糖尿病患者的生活质量。

背景:糖尿病肾病(DN)是糖尿病患者最严重的微血管并发症之一。大约30-40%的糖尿病(DM)患者发展为肾病并进展为肾损伤。它显著降低了糖尿病患者的生活质量。不幸的是,目前的治疗策略仍然不能有效地抑制DN的进展。此外,DN的发病机制尚不清楚。最近的研究表明,肾小管间质纤维化可发生在糖尿病肾病的早期。由于肾小管中含有丰富的线粒体,正常的线粒体功能对功能良好的肾脏至关重要。更重要的是,新出现的证据表明线粒体功能障碍在糖尿病肾病肾小管间质损伤中起关键作用,潜在的改善受损线粒体的新疗法应该对糖尿病肾病有有益的影响。
目的:肾小管间质纤维化是糖尿病肾病(DN)的重要病理特征,肾小管损伤可能与有丝分裂异常有关。本研究旨在探讨AMPK激动剂二甲双胍对糖尿病大鼠肾小管上皮细胞有丝分裂和细胞损伤的影响及其分子机制。
方法:本研究采用高脂饮食(HFD)和链脲佐菌素(STZ)诱导的2型糖尿病小鼠模型和HK-2细胞。二甲双胍口服(200 mg/kg/d)24周。检测肾组织和HK-2细胞的肾小管间质病变、氧化应激和部分吞噬细胞指标(如LC3II、PINK1和Parkin)。此外,应用化合物C(AMPK抑制剂)和PINK1 siRNA探讨了二甲双胍对有丝分裂吞噬的分子调控机制。
结果:我们发现糖尿病小鼠肾组织中p-AMPK、PINK1、Parkin、LC3II和ATG5的表达明显降低。二甲双胍可降低HFD/STZ诱导的糖尿病小鼠的血肌酐、尿蛋白水平,减轻肾脏氧化损伤和纤维化。此外,二甲双胍还逆转了有丝分裂功能障碍和NLRP3的过度表达。体外用AMPK抑制剂化合物C或PINK1 siRNA预处理HK-2细胞可抵消二甲双胍的有利作用。在HG/HFA环境下,二甲双胍激活p-AMPK,促进PINK1从胞浆移位到线粒体,进而促进HK-2细胞有丝分裂的发生。
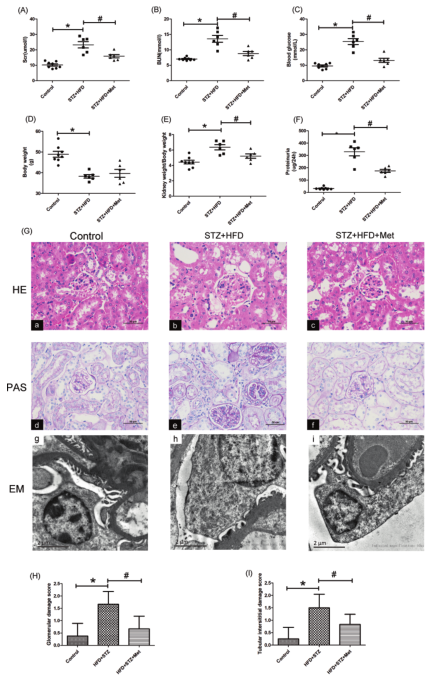
图1 二甲双胍对HFD/STZ糖尿病小鼠肾脏生化指标及肾脏病理改变的影响;A-C观察注射STZ后24周三组小鼠的血清Cr、BUN和血糖水平,D 注射STZ后24周三组小鼠的体重,E 注射STZ后24周三组小鼠的肾重/体重比,F 注射STZ后24周三组小鼠的FT24小时尿蛋白定量。肾组织切片H&E(a-c)和PAS(d-f)染色(放大倍数×400),平均±SD,*P<0.05与对照组,#P<0.05与STZ+HFD组,n=8。电镜分析显示糖尿病小鼠足突融合、肾小球基底膜增厚等超微结构改变。二甲双胍治疗可明显减轻上述损伤。(G-显像化×10,000),n=3。肾小球损伤评分。肾小管-间质损伤评分,*P<0.05与对照组,#P<0.05与STZ+HFD组,n=3。
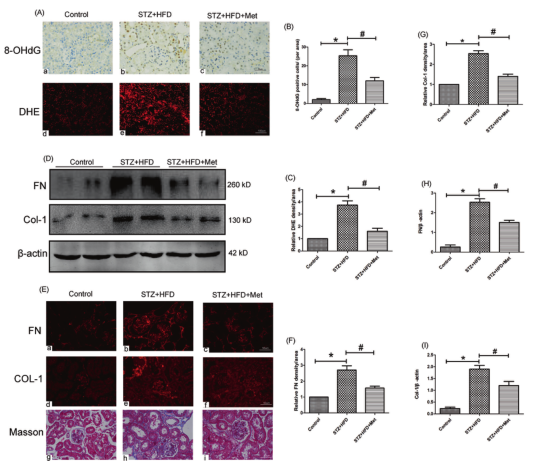
图2 二甲双胍对HFD/STZ糖尿病小鼠肾脏氧化应激和肾间质纤维化的影响;A 3组(放大倍数×200)小鼠肾组织8-OHdG(放大倍率×400,上屏)和DHE染色(下屏)的AIHC分析。B、C,8-OHdG(B)和DHE(C)染色组织的CBar图,*与对照组比较P<0.05,#P<0.05与STZ+HFD组,n=3。D 3组小鼠肾组织FN(上面板)和Col-1(中面板)蛋白表达的DWestern印迹分析:E IF分析3组(放大×400)小鼠肾组织中FN(上面板)和Col-1(中面板)的表达,肾组织切片进行Masson染色(下面板,放大×400)。F、G FN(F)和Col-1(G)的IF染色半定量。免疫印迹结果的H-ID计量学分析,FN为β-肌动蛋白(H),Col-1为β-肌动蛋白(I)。数值表示为平均值±SD,*P<0.05与对照组,#P<0.05与STZ+HFD组,n=3。
结论:我们的结果首次表明AMPK激动剂二甲双胍通过激活p-AMPK-PINK1-Parkin通路激活有丝分裂,从而减轻HFD/STZ诱导的糖尿病小鼠的肾脏氧化应激和肾小管间质纤维化。
原文出处:
Han YC, Tang SQ, Liu YT,et al.AMPK agonist alleviate renal tubulointerstitial fibrosis via activating mitophagy in high fat and streptozotocin induced diabetic mice.Cell Death Dis 2021 Oct 09;12(10)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CEL#
32
#肾小管#
53
#肾小管间质纤维化#
32
#Cell#
29
#Dis#
32
#Death#
28
#高脂#
35
#激动剂#
34