Gastric Cancer:胃食管肿瘤的脑转移:被低估的并发症
2021-07-25 yd2015 MedSci原创
在这个单中心回顾性研究中,GEC患者BRMs的发生率可高达6.5%,且容易发生在男性和腺癌患者中。脑转移手术切除仍可带来生存获益。
胃食管癌(GEC)包括食管、胃食管交界处和胃的上皮性恶性肿瘤,其发病率高且预后较差。而预后较差的常见原因为早期就出现远处转移,多位于肝、肺、骨和腹膜。脑转移是胃肠道肿瘤一种严重的并发症,尤其在上段胃肠道,比如食管癌,胃食管结合部癌和胃癌。目前对其发病率和预后了解较少。有研究报道在过去的25年中,食管癌中脑转移发病率为1.7%,胃癌中脑转移发病率为0.6%。但是,对于胃食管肿瘤中(GEC)脑转移(BRMs)发生的危险因素尚不清楚,从而导致缺乏指导筛查BRMs的相关指南或共识。来自德国的团队开展了相关研究,成果发表在Gastric Cancer杂志上。

该研究2013年1月至2019年12月期间治疗的827例胃食管癌患者。其中54例患者((49.5%)被确认为脑转移(BRMs),最终确认的BRMs的发病率为6.5%。局限期GEC中 BRMs的发生率为5.2% (30/547) ,在晚期GEC患者中发生率为9.8% (24/221) 。54例伴有脑转移患者中,20 例患者初始为局限期(44.4%),34例为晚期患者(55.6%)。
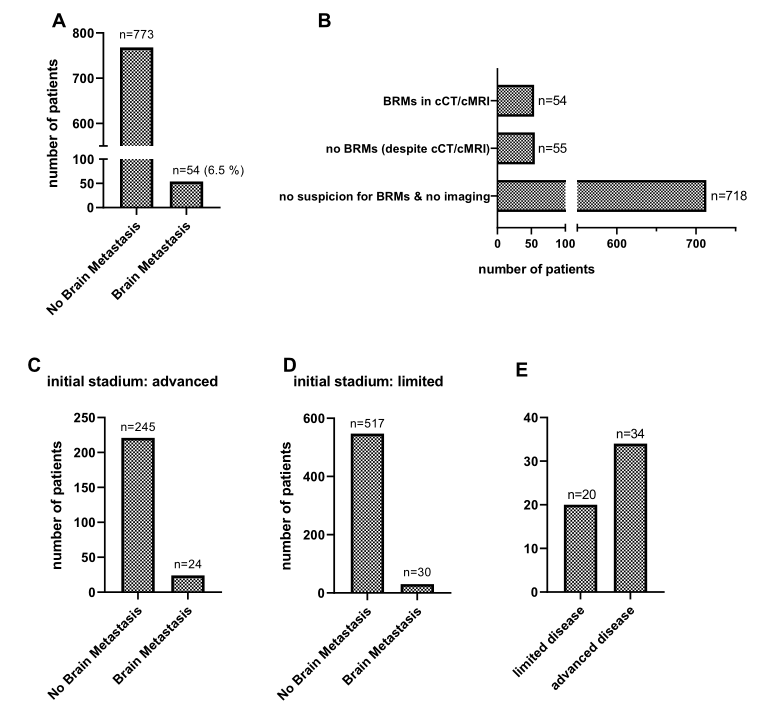
BRMs发病比例比较
BRMs更容易发生在男性患者中(90.74% vs 9.26%, p = 0.0051,RR: 3.251, 95% CI 1.365–7.863)。类似,腺癌患者更容易发生BRMs (90.74% vs 9.26%, p = 0.0117, RR: 2.883, 95% CI 1.213–6.971)。在晚期GEC患者疾病进展过程中BRMs的发生率更高(p = 0.0201)。

BRMs容易发生的亚组
总体人群中,从肿瘤诊断到BRMs出现的中位时间为18.02个月。局限期患者的从肿瘤诊断到BRMs出现的中位时间为20.9个月,而晚期患者的为9.3个月(p = 0.0026)。局限期和晚期GEC伴有BRMs患者的中位生存为16.73个月,而局限期患者伴有BRMs的中位生存为27.37个月,晚期患者只有10.3个月 (p = 0.029)。
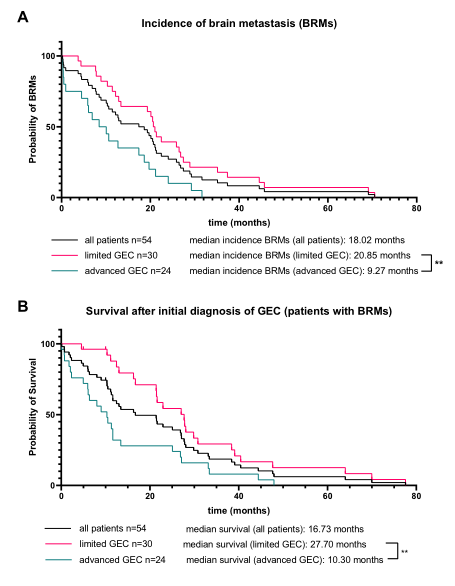
BRMs出现时间和生存
出现BRMs预示着患者预后较差。诊断脑转移后患者的中位生存为3.07个月,局限期和晚期患者出现脑转移后的中位生存没有明显统计学差异(3.185 vs. 2.33个月, p = 0.64)。但是如果脑转移后,能够手术患者对比不能够进行手术患者的中位生存有所延长,有统计学差异(5.93 vs. 2.07个月, p = 0.023)。
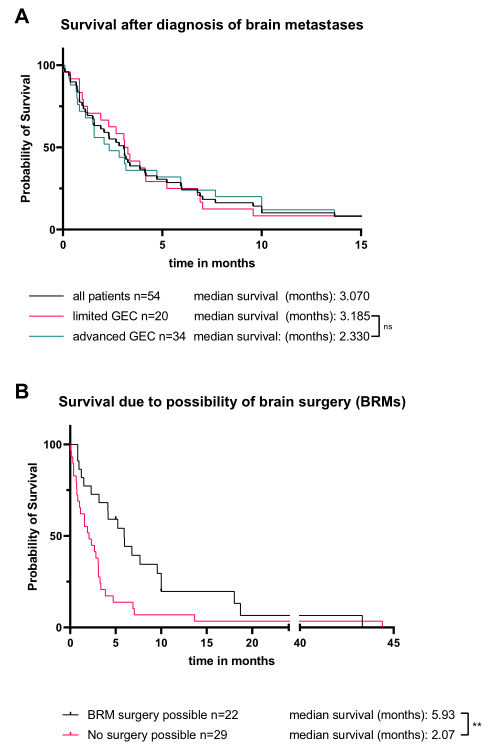
诊断BRMs后的生存
综上,在这个单中心回顾性研究中,GEC患者BRMs的发生率可高达6.5%,且容易发生在男性和腺癌患者中。脑转移手术切除仍可带来生存获益。
原始出处:
Brunner M, Soll D, Adler K, et al. Brain metastases in gastroesophageal cancers-an underestimated complication. Gastric Cancer. 2021 Jul 23. doi: 10.1007/s10120-021-01219-z. Epub ahead of print. PMID: 34297239.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#gastric#
33
#胃食管#
44
#GAS#
39
#食管肿瘤#
45
#并发#
33
#AST#
36
#食管#
33